Solving the Reproducibility Crisis in High-Throughput Screening: Strategies for Robust and Reliable Data
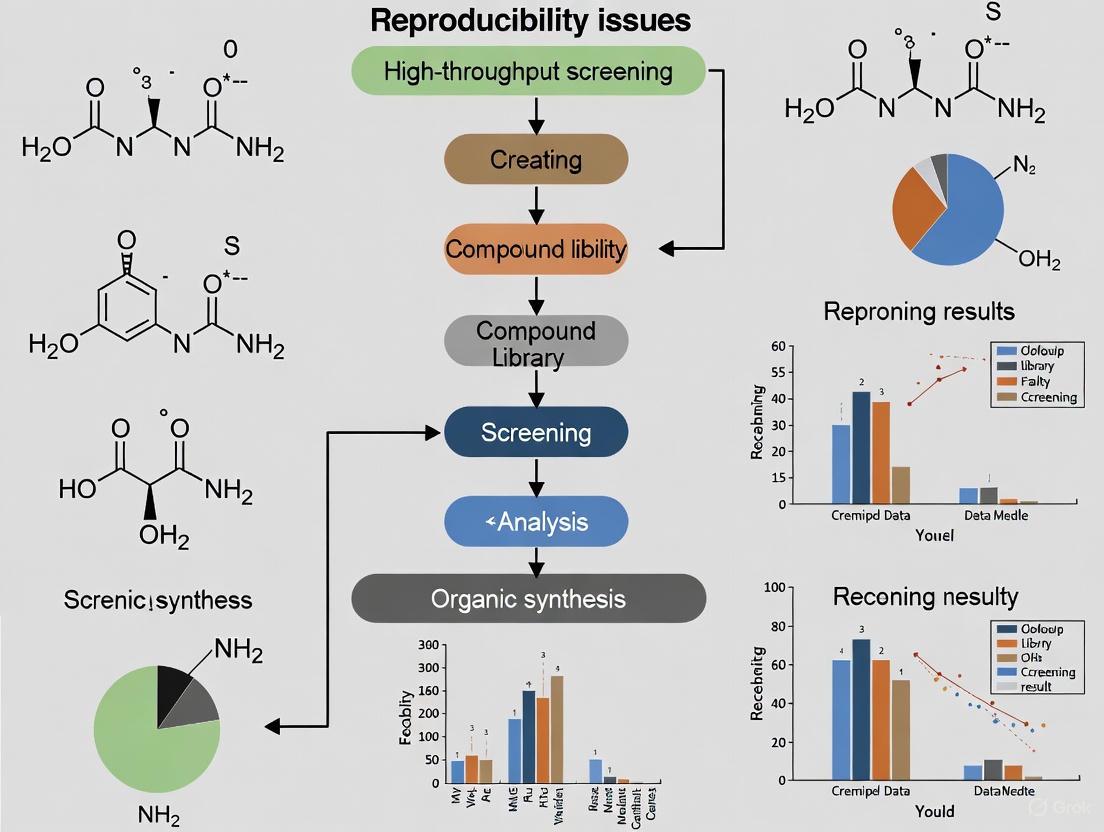
This article addresses the critical challenge of reproducibility in high-throughput screening (HTS), a cornerstone of modern drug discovery and biological research.
Solving the Reproducibility Crisis in High-Throughput Screening: Strategies for Robust and Reliable Data
Abstract
This article addresses the critical challenge of reproducibility in high-throughput screening (HTS), a cornerstone of modern drug discovery and biological research. Aimed at researchers, scientists, and drug development professionals, it provides a comprehensive framework for understanding, mitigating, and validating HTS workflows to ensure data robustness. We first explore the foundational causes of irreproducibility, from technical variability to environmental factors. The discussion then progresses to methodological solutions, including advanced automation and rigorous assay design. A dedicated troubleshooting section offers practical optimization strategies, while the final segment details robust validation protocols and comparative analyses of technologies and reagents. By synthesizing these four intents, this guide empowers scientists to implement reproducible HTS practices, thereby accelerating the development of reliable scientific discoveries and therapeutics.
Understanding the Roots of Irreproducibility in HTS
Defining Reproducibility, Repeatability, and Reliability in an HTS Context
In modern drug discovery, High-Throughput Screening (HTS) serves as a critical tool for rapidly testing large libraries of chemical or biological compounds against specific therapeutic targets [1]. The core value of any HTS campaign lies in the confidence of its results, making reproducibility, repeatability, and reliability foundational concepts. These are not merely academic concerns; issues with reproducibility have reached alarming rates in preclinical research, with studies indicating that 50% to 80% of published results may not be reproducible [2]. This irreproducibility represents not just a scientific challenge but also a significant economic burden, estimated to account for approximately $28 billion in spent funding in the U.S. alone for preclinical research that cannot be reproduced [2].
Within the HTS workflow, these terms carry specific technical meanings. Reproducibility typically refers to the consistency of results across different replicates, experiments, or laboratories. Repeatability often concerns the consistency of measurements under identical, within-laboratory conditions. Reliability encompasses the overall trustworthiness of the data, indicating that results are robust, reproducible, and minimize false positives and negatives. Understanding and optimizing these parameters is essential because HTS activities consume substantial resources—utilizing large quantities of biological reagents, screening hundreds of thousands to millions of compounds, and employing expensive equipment [3]. Before embarking on full HTS campaigns, researchers must therefore validate their processes to ensure the quality and reproducibility of their outcomes [3].
Troubleshooting Guides for HTS Reproducibility
Addressing Variability and Human Error
Problem: High inter- and intra-user variability in manual processes leads to inconsistent results.
Solution: Implement automated workflows to standardize procedures.
- Liquid Handling Automation: Utilize non-contact dispensers and robotic systems to eliminate pipetting variability. Systems equipped with verification technology (e.g., DropDetection) can confirm that correct liquid volumes have been dispensed into each well, allowing errors to be identified and corrected [4].
- Assay Miniaturization: Transition to 384-well or 1536-well plates to reduce reagent consumption and variability while increasing throughput. This miniaturization can reduce reagent consumption and overall costs by up to 90% [4].
- Workflow Integration: Employ integrated robotic platforms that handle multiple plates consistently, reducing human intervention and associated errors [4] [5].
Validation Metric: Monitor the coefficient of variation (CV) across replicate wells. A CV below 10-15% typically indicates acceptable pipetting precision in automated systems.
Managing Missing Data and Dropouts
Problem: High levels of missing observations, common in techniques like single-cell RNA-seq, skew reproducibility assessments [6].
Solution: Apply statistical methods designed to handle missing data.
- Latent Variable Models: Use advanced statistical approaches like correspondence curve regression (CCR) with latent variables to incorporate information from missing values rather than excluding them [6].
- Threshold-Based Assessment: Evaluate consistency across a series of rank-based selection thresholds rather than relying solely on correlation measures that require complete data [6].
- Data Imputation Validation: When using imputation methods, validate them with pilot studies that intentionally mask known data points to assess imputation accuracy.
Validation Metric: Compare Spearman correlation with and without zero-count transcripts. Significant differences indicate potential missing data bias [6].
Overcoming Data Handling Challenges
Problem: Vast volumes of multiparametric data create analysis bottlenecks and obscure meaningful patterns.
Solution: Implement specialized HTS software and data management systems.
- Integrated HTS Platforms: Utilize software that combines assay setup, plate design, instrument integration, and downstream data analysis in a unified system [7].
- Automated QC Checks: Deploy AI-driven quality control systems that automatically flag outliers, technical errors, and plate-level artifacts [7].
- Standardized Analysis Pipelines: Develop consistent data normalization and transformation protocols that are applied across all screens to minimize analytical variability.
Validation Metric: Track Z'-factor across plates (0.5-1.0 indicates excellent assay robustness) [8]. Consistent Z' values indicate stable data quality.
Optimizing Assay Design and Validation
Problem: Poorly designed assays generate false positives and negatives, compromising reliability.
Solution: Implement rigorous assay development and validation protocols.
- Orthogonal Assays: Confirm primary screening hits using different detection technologies or assay formats to eliminate technology-specific artifacts [9].
- Counter-Screening: Identify and filter out compounds with undesirable mechanisms of action (e.g., auto-fluorescent compounds in fluorescence-based assays) [9].
- Pilot Studies: Conduct small-scale pilot experiments to validate assay performance before full implementation [9].
Validation Metric: Establish a multi-tiered confirmation cascade: primary screen → confirmatory screening → dose-response → orthogonal testing → secondary screening [9].
Table 1: Key Performance Metrics for HTS Assay Validation
| Metric | Target Value | Interpretation |
|---|---|---|
| Z'-factor | 0.5 - 1.0 | Excellent assay robustness [8] |
| Signal-to-Noise Ratio | >5 | Sufficient detection sensitivity [8] |
| Coefficient of Variation (CV) | <10-15% | Acceptable well-to-well precision |
| Signal Window | >2-fold | Adequate dynamic range [8] |
Statistical Assessment of Reproducibility
Reproducibility Indexes and Measures
Statistical assessment is crucial for quantifying HTS reproducibility. Multiple methods exist, each with strengths and limitations:
- Correspondence Curve Regression (CCR): This method models how the probability that a candidate consistently passes selection thresholds in different replicates is affected by operational factors. It evaluates reproducibility across a series of rank-based thresholds, providing a comprehensive view beyond single-threshold measures [6].
- Irreproducible Discovery Rate (IDR): A method that profiles how consistently candidates are ranked and selected in replicate experiments across a sequence of selection thresholds [6].
- Spearman/Pearson Correlation: Traditional measures of association between replicate measurements. However, these can yield conflicting results when missing data handling approaches differ, making them potentially misleading without complementary measures [6].
The following diagram illustrates the statistical assessment workflow for evaluating reproducibility in HTS:
Incorporating Missing Data in Reproducibility Assessment
Standard reproducibility measures often fail when substantial missing data exists due to underdetection, as commonly occurs in single-cell RNA-seq where many genes report zero expression levels [6]. A principled approach accounts for these missing values:
- Latent Variable Approach: Extends statistical models like CCR to incorporate candidates with unobserved measurements, providing more accurate reproducibility assessments [6].
- Comparative Analysis: Evaluate how different missing data treatments affect reproducibility conclusions. For example, in a study of HCT116 cells, TransPlex kits showed lower Spearman correlation (0.648) than SMARTer kits (0.734) when zeros were included, but the opposite pattern emerged when only non-zero transcripts were considered [6].
Table 2: Impact of Missing Data Handling on Reproducibility Metrics
| Analysis Method | TransPlex Kit | SMARTer Kit | Conclusion |
|---|---|---|---|
| Spearman (zeros included) | 0.648 | 0.734 | SMARTer more reproducible [6] |
| Spearman (non-zero only) | 0.501 (8,859 transcripts) | 0.460 (6,292 transcripts) | TransPlex more reproducible [6] |
| Pearson (zeros included) | Higher | Lower | TransPlex more reproducible [6] |
| Pearson (non-zero only) | Higher | Lower | TransPlex more reproducible [6] |
Frequently Asked Questions (FAQs)
Q1: What is the difference between reproducibility and repeatability in HTS?
A: In HTS context, repeatability typically refers to the consistency of results when the same experiment is performed multiple times under identical conditions (same operator, equipment, and short time interval). Reproducibility refers to the consistency of results when experiments are conducted under changing conditions (different operators, equipment, or laboratories) [3] [6]. Both are components of overall reliability, which encompasses the trustworthiness of data throughout the screening cascade.
Q2: How can we distinguish between true hits and false positives in HTS?
A: True hits can be distinguished through a multi-stage confirmation process: (1) Confirmatory screening retests active compounds using the same assay conditions; (2) Dose-response screening determines potency (EC50/IC50) across a concentration range; (3) Orthogonal screening uses different technologies to confirm target engagement; (4) Counter-screening identifies compounds with interfering properties; (5) Secondary screening confirms biological relevance in functional assays [9].
Q3: What are the most critical factors for achieving reproducible HTS results?
A: The most critical factors include: (1) Assay robustness with Z'-factor >0.5 [8]; (2) Automated liquid handling to minimize human error [4]; (3) Proper statistical handling of missing data [6]; (4) Standardized operating procedures across users and sites [4]; (5) Quality compound libraries with documented purity and solubility [9].
Q4: How does automation specifically improve HTS reproducibility?
A: Automation enhances reproducibility by: (1) Reducing human error in repetitive tasks; (2) Standardizing liquid handling across users and experiments; (3) Enabling miniaturization which reduces reagent-based variability; (4) Providing verification features (e.g., drop detection) to confirm proper dispensing [4].
Q5: What statistical measures are most appropriate for assessing HTS reproducibility?
A: The appropriate measure depends on your data characteristics: (1) Correspondence curve methods are ideal for rank-based data with multiple thresholds [6]; (2) Z'-factor assesses assay robustness (0.5-1.0 indicates excellent assay) [8]; (3) Correlation coefficients (Spearman/Pearson) are common but can be misleading with missing data [6]; (4) CV (coefficient of variation) measures precision across replicates.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for HTS Reproducibility
| Reagent/Equipment | Function | Reproducibility Consideration |
|---|---|---|
| Non-Contact Liquid Handlers | Precise reagent dispensing without cross-contamination | Drop detection technology verifies dispensed volumes [4] |
| 384-/1536-Well Microplates | Miniaturized assay formats | High-quality plates with minimal well-to-well variability ensure consistent results [5] |
| Validated Compound Libraries | Collections of chemically diverse screening compounds | Well-curated libraries with known purity and solubility reduce false results [9] |
| Transcreener ADP² Assay | Universal biochemical assay for multiple targets | Flexible design allows testing multiple targets with same detection method [8] |
| Cell Line Authentication | Verified cellular models for screening | Authenticated, low-passage cells ensure physiological relevance and consistency [5] |
| QC-Ready Detection Reagents | Fluorescence, luminescence, or absorbance detection | Interference-resistant readouts minimize false positives [8] |
Experimental Protocol: Implementing a Reproducibility Assessment Framework
Step-by-Step Methodology
To systematically evaluate and improve reproducibility in your HTS workflow, follow this detailed protocol:
Assay Development and Miniaturization
- Develop your assay in a 96-well format first, optimizing biological and detection parameters.
- Miniaturize to 384-well or 1536-well format, maintaining key performance metrics (Z' > 0.5, signal-to-noise > 5) [8].
- Validate miniaturized assay with positive and negative controls across at least 3 independent runs.
Automated Workflow Implementation
- Program liquid handlers for consistent reagent dispensing across all plates.
- Implement real-time dispensing verification if available (e.g., DropDetection technology) [4].
- Establish standardized plate handling procedures to minimize edge effects and evaporation.
Pilot Screening and Statistical Power Analysis
- Conduct a pilot screen with 5-10% of the compound library in replicate.
- Calculate statistical power and determine appropriate replicate number based on effect size and variability.
- Use correspondence curve regression or similar methods to assess preliminary reproducibility [6].
Full-Scale Screening with Embedded Controls
- Distribute positive and negative controls across all plates to monitor inter-plate variability.
- Include randomized compound placement to avoid positional bias.
- Implement periodic quality checks with standardized acceptance criteria.
Data Analysis and Hit Confirmation
The following workflow diagram illustrates the comprehensive HTS process with quality control checkpoints:
This experimental protocol emphasizes continuous quality monitoring at each stage, enabling researchers to identify and address reproducibility issues proactively throughout the HTS campaign.
Troubleshooting Guides
Instrumentation and Data Quality Control
Issue: How can I identify systematic spatial artifacts in my high-throughput screening (HTS) plates that traditional quality control methods miss?
Traditional control-based quality control (QC) metrics like Z-prime (Z'), SSMD, and signal-to-background ratio (S/B) are industry standards but have a fundamental limitation: they can only assess the fraction of the plate containing control wells and cannot detect systematic errors affecting drug wells [10]. These undetected spatial artifacts—such as evaporation gradients, systematic pipetting errors, temperature-induced drift, or column-wise striping—can significantly compromise data reproducibility [10].
Solution: Implement the Normalized Residual Fit Error (NRFE) metric alongside traditional QC methods. NRFE evaluates plate quality directly from drug-treated wells by analyzing deviations between observed and fitted dose-response values, accounting for response-dependent variance [10].
Protocol for NRFE-based Quality Control:
- Perform Dose-Response Experiment: Conduct your HTS experiment as planned, ensuring drug treatments span multiple concentrations.
- Calculate Traditional QC Metrics: Compute Z-prime (Z' > 0.5), SSMD (>2), and S/B ratio (>5) from control wells to capture assay-wide technical issues [10].
- Fit Dose-Response Curves: Generate fitted dose-response curves for all compounds on the plate.
- Compute NRFE: Calculate the NRFE metric, which is based on the deviations (residuals) between the observed data points and the fitted curve, normalized by a binomial scaling factor [10].
- Apply Quality Thresholds: Use the following tiered system to classify plate quality [10]:
- NRFE < 10: Acceptable quality.
- NRFE 10-15: Borderline quality; requires additional scrutiny.
- NRFE > 15: Low quality; exclude from analysis or carefully review.
Plates flagged by high NRFE exhibit substantially lower reproducibility among technical replicates. Integrating NRFE with traditional QC can improve cross-dataset correlation and overall data reliability [10].
Reagent Variability and Quality Assurance
Issue: How do I mitigate lot-to-lot variance (LTLV) in immunoassays and other reagent-dependent assays?
Lot-to-lot variance is a significant challenge, negatively impacting assay accuracy, precision, and specificity. It is estimated that 70% of an immunoassay's performance is attributed to the quality of raw materials, while the remaining 30% depends on the production process [11]. Fluctuations in key biologics like antibodies, antigens, and enzymes are primary contributors.
Solution: Implement rigorous quality control and validation procedures for all critical reagents.
Protocol for Managing Reagent LTLV:
- Thorough Reagent Evaluation: Before adopting a new reagent lot, assess its critical quality attributes.
- For Antibodies and Antigens: Evaluate activity, concentration, affinity, specificity, purity, and stability. Use SDS-PAGE, SEC-HPLC, or capillary electrophoresis to check for aggregates and impurities, which can cause high background or inaccurate readings [11].
- For Enzymes (e.g., HRP, ALP): Confirm enzymatic activity units, not just purity. Be aware that purity of 90-95% is often acceptable, but the biological activity of impurities can vary [11].
- Perform Bridging Experiments: When a new lot is received, run parallel assays using both the old and new lots on the same set of characterized samples. This directly compares performance and identifies any significant shift in results.
- Use a Master Calibrator and QC Panel: Maintain a stable, well-characterized master calibrator and quality control panel to benchmark the performance of new reagent lots against a consistent standard [11].
- Document Everything: Keep detailed records of all reagent lots, including certificates of analysis, quality control data, and performance validation results from bridging studies.
Environmental Factors and Laboratory Conditions
Issue: What are the primary environmental factors that introduce variability, and how can they be controlled?
Laboratories are sensitive environments where minor variations in conditions can dramatically affect experimental outcomes, sample integrity, and instrument performance [12]. Key factors include temperature, humidity, air quality, and physical disturbances like vibration and noise.
Solution: Proactively monitor and control the laboratory environment using appropriate instruments and established protocols.
Protocol for Environmental Monitoring and Control:
- Temperature: Maintain a general lab temperature of 20–25°C (68–77°F), with tighter control for specific applications. Use digital temperature monitors with alarms to track conditions in the lab, as well as in refrigerators, incubators, and other storage units [12].
- Humidity: Control relative humidity between 30-50% to prevent microbial growth and corrosion (high humidity) or static electricity buildup (low humidity). Use hygrometers to monitor levels and employ dehumidifiers or humidifiers as needed [12].
- Air Quality: Ensure adequate ventilation, typically 6-12 air changes per hour, to protect against contaminants. Use high-efficiency air filters and monitor air quality with meters that can detect CO2 and other particulates [12].
- Pipette Performance: Account for environmental effects on liquid handling, which is a major source of error.
- Altitude/Barometric Pressure: Pipettes under-deliver at high altitudes due to lower air density. Calibrate pipettes in the environment where they are used, or adjust the delivery setting to compensate for the repeatable error [13].
- Thermal Disequilibrium: Pipettes over-deliver cold liquids and under-deliver warm liquids. To minimize error, pre-equilibrate liquids and pipettes to the same temperature, minimize the time the tip is exposed to a different temperature, and pipette close to the maximum volume where practical [13].
The following table summarizes the impact of these factors and solutions:
| Environmental Factor | Impact on Experiments | Ideal Range | Control Solution |
|---|---|---|---|
| Temperature | Alters reaction rates; degrades samples; affects instrument calibration [12]. | 20–25°C (68–77°F) [12] | Digital temperature monitors; calibrated storage units [12]. |
| Humidity | Causes sample contamination/corrosion (high); static electricity (low) [12]. | 30-50% Relative Humidity [12] | Hygrometers; dehumidifiers/humidifiers; desiccants for storage [12]. |
| Air Quality | Leads to sample contamination; equipment damage; health hazards [12]. | 6-12 air changes/hour [12] | High-efficiency air filters; air quality meters (CO2, particles) [12]. |
| Pipetting (Altitude) | Volume under-delivery at high altitude [13]. | N/A | Calibrate pipettes in-lab; adjust delivery settings [13]. |
| Pipetting (Liquid Temp.) | Over-delivery of cold liquid; under-delivery of warm liquid [13]. | Liquid temp. = Pipette temp. | Pre-equilibrate liquids; use rapid, consistent technique [13]. |
Frequently Asked Questions (FAQs)
Q: My experimental results are inconsistent between replicates. What should be my first step in troubleshooting? A: The first step is often to repeat the experiment. Simple, unintentional mistakes can occur. If the problem persists, systematically review your assumptions, methods, and controls. Ensure all equipment is calibrated, reagents are fresh and stored correctly, and you have included appropriate positive and negative controls [14] [15].
Q: I have a dim fluorescent signal in my immunohistochemistry experiment. What are the most common causes? A: A dim signal could indicate a problem with the protocol, but also consider the biological context—the protein may simply not be highly expressed in that tissue. Technically, check that your reagents have not degraded, your primary and secondary antibodies are compatible, and you have not over-fixed the tissue or used antibody concentrations that are too low. Change one variable at a time, starting with the easiest, such as adjusting microscope settings [14].
Q: How can I improve the overall reproducibility of my high-throughput screening process? A: Beyond specific troubleshooting, focus on process validation. Before a full HTS campaign, run a validation study to optimize the workflow and statistically evaluate the assay's ability to distinguish active from non-active compounds robustly. Utilize a variety of reproducibility indexes to benchmark performance [3].
Q: What is the most overlooked source of pipetting error? A: Thermal disequilibrium—pipetting liquids that are at a different temperature than the pipette itself—is a major and often overlooked source of error that can cause over- or under-delivery by more than 30%. Always equilibrate your liquids and pipette to room temperature for critical volume measurements [13].
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function | Key Consideration |
|---|---|---|
| High-Quality Antibodies | Specific detection of target proteins or analytes in assays. | Monitor for aggregates and impurities via SEC-HPLC; test for activity and specificity with each new lot [11]. |
| Characterized Antigens | Serve as calibrators, controls, or targets in immunoassays. | Assess purity (e.g., via SDS-PAGE) and stability; ensure appropriate storage buffers are used [11]. |
| Enzymes (HRP, ALP) | Used as labels for detection in colorimetric, fluorescent, or chemiluminescent assays. | Quality should be measured in activity units, not just purity; source from reliable manufacturers [11]. |
| Assay Buffers & Diluents | Provide the chemical environment for the reaction. | Must be mixed thoroughly; variations in pH or conductivity can significantly affect assay performance [11]. |
| Solid Phases (Microplates, Magnetic Beads) | Provide the solid support for assay reactions. | Ensure consistency in coating, binding capacity, and low non-specific binding across lots [11]. |
Experimental Workflow and Troubleshooting Logic
The following diagram illustrates a systematic workflow for troubleshooting experiments, integrating checks for instrumentation, reagents, and environmental factors.
Quality Control Integration in HTS
This diagram shows how different quality control methods provide complementary oversight in high-throughput screening.
FAQs: Photoreactor Design and Reproducibility
Q1: Why is my photocatalytic reaction failing when I follow a published procedure exactly?
A: Even with identical chemical ingredients, small changes in your physical setup can cause failure. Key parameters often omitted from publications include [16] [17]:
- Photon Flux and Spectrum: The light source's intensity (W/m²) and spectral output (peak wavelength & FWHM) are critical but rarely fully characterized in methods sections [16] [17].
- Reaction Temperature: Light sources emit heat, and internal photochemical processes can significantly raise the reaction mixture's temperature, leading to unproductive side reactions. Reported cooling methods (e.g., "a fan was used") are often insufficient; the internal reaction temperature is what matters [16] [17].
- Vessel Geometry and Irradiation Path Length: Due to the high extinction coefficients of photocatalysts, light often penetrates only the first few millimeters of the reaction mixture. The vessel's shape and diameter dramatically affect how much reaction volume is effectively irradiated [16] [17].
Q2: What are the advantages of commercial photoreactors over homemade setups?
A: Commercial reactors are engineered to control the variables that undermine reproducibility [18] [19]:
- Uniform Irradiation: They provide even, consistent light distribution to all samples, which is extremely difficult to achieve with homemade LED arrays [18] [19].
- Integrated Temperature Control: They actively manage the heat generated by the light source, maintaining a consistent temperature across all reaction vessels [18].
- Standardized Geometry: They fix the distance between the light source and the reaction vial, a key variable affecting light intensity [16] [18].
- Safety and Ease of Use: They incorporate safety features (e.g., interlock switches) and are designed for user-friendly operation [19].
Q3: How can I improve reproducibility in high-throughput photocatalysis screening?
A: The core challenge is ensuring uniform conditions across all positions in a parallel reactor [16].
- Validate Your Reactor: Perform a "homogeneity test" by running the same model reaction in every well of the plate and analyzing the outcomes. Significant variations indicate underlying problems with light or temperature uniformity [16].
- Control Stirring/Shaking: Efficient and consistent mixing is crucial to overcome mass transfer limitations and ensure all reaction volume is exposed to light [16].
- Report Specifications: When publishing, include the technical specs of the parallel photoreactor and the results of uniformity tests. This provides immense value to the community [16].
Q4: My reaction works well in batch but fails during scale-up in flow. What could be wrong?
A: While flow reactors often provide superior irradiation, new failure points emerge [16] [17]:
- Fraction Collection Timing: In flow chemistry, the product is collected over time. If collection occurs outside the window of "steady-state" conditions, the product can be diluted, leading to highly variable results and yields [16] [17].
- Irradiation Path Length: Simply scaling a flow reaction by increasing the reactor diameter can be detrimental because light cannot penetrate as deeply into the center of the wider tube, leaving some substrate unreacted [16] [17].
Troubleshooting Guide
This guide helps diagnose and solve common photoreproducibility issues.
Table: Troubleshooting Photochemical Reactions
| Symptom | Possible Cause | Recommended Solution |
|---|---|---|
| Low or inconsistent yield between identical runs | Inhomogeneous irradiation; Inconsistent temperature; Poor mass transfer | Use a reactor with even light distribution and active cooling; Ensure efficient stirring; Characterize light source intensity and spectrum [16] [18] [17]. |
| Reaction works in a small vial but fails upon scaling up | Increased irradiation path length; Inefficient light penetration | Switch to a continuous flow reactor or a scaled batch reactor designed to maintain a short light path length [16] [17] [19]. |
| Variable results across positions in a parallel reactor | Non-uniform light field across the plate; Position-dependent temperature differences | Validate reactor homogeneity by running the same reaction in every well; Use a reactor designed for uniform parallel processing [16]. |
| Formation of different or unexpected byproducts | Uncontrolled temperature leading to thermal side reactions | Implement better temperature control of the reaction mixture itself, not just the reactor block [16] [17]. |
| Reaction fails to reproduce a literature procedure | Undisclosed critical parameter (e.g., photon flux, vial type, distance to light source) | Consult literature on reproducibility; Contact the original authors for details; Use a standardized, well-characterized commercial reactor [16] [18] [17]. |
Experimental Protocols for Ensuring Reproducibility
Protocol 1: Validating Homogeneity in a Parallel Photoreactor
Purpose: To verify that all reaction positions within a high-throughput photoreactor experience identical conditions, ensuring data robustness [16].
Materials:
- Parallel photoreactor (e.g., EvoluChem PhotoRedOx Box, Illumin8) [18] [19].
- Standardized reaction vial type (e.g., 2 mL HPLC vials).
- Model photochemical reaction mixture (e.g., Photomethylation of buspirone) [18].
Methodology:
- Preparation: Prepare a large, homogeneous master mix of your model reaction.
- Loading: Dispense equal aliquots of the reaction mixture into vials and place them in every available position of the reactor.
- Irradiation: Run the photochemical reaction for a set time that achieves moderate conversion (e.g., 30-70%). This helps identify kinetic differences more clearly than at full conversion [16].
- Analysis: Quench and analyze each reaction vial using a standardized quantitative method (e.g., UPLC, GC).
- Data Analysis: Calculate the average conversion and the standard deviation across all positions.
Interpretation: A low standard deviation (e.g., ±2% as demonstrated in one study [18]) indicates a homogeneous reactor. Significant outliers or trends across the plate flag issues with light or temperature uniformity [16].
Protocol 2: Characterizing a Photochemical Reaction for Publication
Purpose: To document all critical parameters required for another lab to successfully reproduce a photochemical reaction.
Materials:
- Photoreactor
- Light meter (for intensity)
- Spectrometer (for emission spectrum)
- Temperature probe (for internal reaction temperature)
Methodology: Report the following parameters in the experimental section [16] [17]:
- Light Source: Manufacturer, model, and wavelength (e.g., "Kessil PR160L 440 nm"). Include the spectral output (peak & FWHM) and optical power or intensity (W/m² or mW/cm²) at the reaction vessel.
- Reactor Setup: Type (batch/flow), manufacturer, and model. For batch, specify the vessel type (e.g., "20 mL scintillation vial"), material (e.g., "borosilicate glass"), and the distance from the light source.
- Temperature Control: Method of cooling (e.g., "cooling fan") and, crucially, the measured temperature of the reaction mixture during irradiation.
- Mixing: Stirring speed (RPM) or shaking frequency.
- Atmosphere: Reaction atmosphere (e.g., "degassed with N₂ for 5 minutes" or "sealed under air").
Research Reagent Solutions & Essential Materials
Table: Key Components for Reproducible Photocatalysis
| Item | Function | Key Considerations |
|---|---|---|
| Standardized LED Light Source | Provides photons to excite the photocatalyst. | Narrow emission band (FWHM), stable power output, commercial availability. Wavelength and intensity must be reported [16] [17] [19]. |
| Photocatalyst (e.g., Ir(dF(CF₃)ppy)₂(dtbpy)PF₆) | Absorbs light and mediates electron transfer events. | Should be commercially available or easily synthesized. High purity is essential [18] [17]. |
| Temperature-Controlled Photoreactor | Houses the reaction and manages heat. | Active cooling (e.g., Peltier, fan), even light distribution, and compatibility with standard vial formats [18] [19]. |
| Vial Set (0.3 mL to 20 mL) | Holds the reaction mixture. | Material (e.g., glass transmissivity), geometry, and sealing method can impact the reaction [18]. |
| Inert Atmosphere System | Controls the reaction environment. | Prevents inhibition by oxygen or other atmospheric gases. Details on degassing procedure should be reported [16] [17]. |
Supporting Diagrams
Diagram: Troubleshooting Photoreproducibility Workflow
Diagram: Protocol for Reactor Validation
Why Biological Complexity and Unique Dataset Patterns Challenge Validity
Frequently Asked Questions
Q: What are the most common sources of poor reproducibility in high-throughput behavioral screens? A: The primary sources are often biological and technical. Biologically, slight variations in organism health, age synchronization, or culture conditions can introduce significant noise. Technically, insufficient statistical power from low replicate numbers, over-reliance on manual feature selection, and assays that are not robust enough for automation can lead to findings that fail to validate [20].
Q: How can I make the data visualizations from my screening results accessible and interpretable for all team members? A: Adopt accessible data visualization practices. This includes providing a text summary of the key trends, ensuring a contrast ratio of at least 3:1 for graphical elements and 4.5:1 for text, and not using color as the only way to convey information. Supplement charts with accessible data tables and use simple, direct labeling instead of complex legends [21] [22] [23].
Q: Our AI models identify promising compounds, but they often fail in subsequent biological validation. Are we using the wrong models? A: Not necessarily. This often highlights a disconnect between the computational prediction and biological reality. AI models are only as good as the data they are trained on. The failure may stem from a lack of robust, physiologically relevant functional assay data to train the models effectively. AI-generated "informacophores" must be rigorously validated through empirical biological assays to confirm therapeutic potential [24].
Q: Why would a machine learning model outperform traditional statistical methods in analyzing complex phenotypic data? A: Traditional statistical methods, like t-tests with multiple comparison corrections, can have low statistical power for detecting subtle, non-linear patterns. They generate binary results (significant/not significant) and are designed for linear relationships. Machine learning models, such as Random Forests, can capture these complex, non-linear interactions between multiple features, providing a more quantitative and robust measure of treatment effects [20].
Troubleshooting Guides
Problem: High Variability in Model Organism Behavior
Issue: Your C. elegans or other model organism screens show high levels of behavioral variability, making it difficult to distinguish true treatment effects from noise.
Solution:
- Standardize Culture Conditions: Implement strict protocols for organism age synchronization, temperature, and food source to minimize pre-analytical variability.
- Increase Replication: Ensure an adequate number of biological replicates are used to account for inherent biological variation. Do not rely on a small number of wells or plates.
- Automate Data Collection: Use automated tracking platforms (e.g., Tierpsy Tracker) to reduce observer bias and consistently extract a large number of morphological and movement features [20].
- Validate with ML: Train a machine learning classifier (e.g., Random Forest) to distinguish between control and disease-model strains as a quality control step before proceeding with drug screening. A high-performing model confirms that the phenotypic difference is detectable [20].
Problem: Inaccessible or Misleading Data Visualizations
Issue: Colleagues or reviewers misinterpret your charts, or the charts are not accessible to individuals with color vision deficiencies.
Solution:
- Provide Multiple Formats: Always accompany a chart with a text summary describing the key trends and a link to an accessible data table [21] [22].
- Check Contrast: Use tools like the WebAIM Contrast Checker to ensure all elements meet WCAG guidelines: at least 3:1 for graphics and 4.5:1 for text [22] [23].
- Go Beyond Color: Use a combination of color, patterns, shapes, and direct data labels to convey information. This ensures understanding is not dependent on color perception alone [21] [25].
- Use Accessible Palettes: When building custom tools, leverage established, accessible color palettes from libraries like D3.js (e.g.,
schemeDark2,schemeSet3) which are designed for categorical differentiation [26] [27].
Problem: Translating AI-Hit Compounds to Biologically Relevant Leads
Issue: Compounds identified through AI-powered virtual screening do not show efficacy in functional biological assays.
Solution:
- Focus on Data Quality: "Garbage in, garbage out" is a key principle. AI models require high-quality, well-annotated training data. Invest in generating robust biological assay data with complete metadata [28] [24].
- Implement a Feedback Loop: Create an iterative cycle where AI predictions are validated through wet-lab experiments, and the experimental results are fed back to refine and retrain the AI models [24].
- Use Relevant Assays: Employ biologically relevant functional assays (e.g., high-content screening, 3D cell cultures) that can capture complex phenotypic changes and provide a more translational readout [24].
- Prioritize Explainability: Where possible, use machine learning models that offer some level of interpretability (e.g., Random Forest) to understand which features are driving the predictions, or use hybrid models that combine AI with medicinal chemistry intuition [20] [24].
Experimental Protocols & Data
Machine Learning-Based Phenotypic Screening Protocol
This protocol outlines a method for using machine learning to analyze high-throughput behavioral data from C. elegans, offering a more sensitive alternative to traditional statistical tests [20].
Strain Preparation & Video Acquisition:
- Culture control (e.g., N2) and disease-model strains of C. elegans under standardized conditions.
- For drug screening, treat disease-model worms with compounds from your library.
- Using an automated capture system, record videos of worms in multi-well plates. Include a period with a specific stimulus (e.g., blue light pulses) to elicit measurable behavioral responses.
Feature Extraction:
- Process the videos using tracking software like Tierpsy Tracker.
- The software will extract a large set of quantitative features for each worm trajectory, including speed, morphology (length, curvature), and movement patterns.
- Average the features from all trajectories within a single well to generate a single feature vector per well.
Model Training & Validation:
- Use the feature vectors from control and disease-model strains (untreated) to train a classifier, such as a Random Forest.
- Reserve a portion of this data as a validation set to confirm the model can accurately distinguish between the two strains.
Drug Efficacy Scoring (Recovery Index):
- Input the feature vectors from drug-treated disease-model worms into the trained classifier.
- Use the classifier's output confidence score as a Recovery Index. A higher confidence score assigned to the "control" class indicates a stronger treatment effect, representing the percentage of phenotypic recovery towards the wild-type state.
Quantitative Data from ML vs. Statistical Methods
The table below summarizes a comparison of approaches for analyzing a drug repurposing screen in C. elegans, highlighting the advantages of ML [20].
| Method | Number of Features Analyzed | Key Limitation | Result on Test Dataset |
|---|---|---|---|
| Traditional Statistics (Block permutation t-test) | 3 core features selected manually | Low power after multiple-test correction; fails to detect subtle, non-linear patterns. | No hits detected when analysis was expanded to 256 features. |
| Machine Learning (Random Forest) | All 256 features simultaneously | Higher computational cost; requires careful validation to prevent overfitting. | Identified compounds with a significant recovery effect by capturing complex patterns. |
Research Reagent Solutions
Essential materials and tools for implementing a robust, high-throughput screening pipeline.
| Item | Function / Explanation |
|---|---|
| Tierpsy Tracker | Open-source software used to automatically track worms in videos and extract a high-dimensional set of morphological and movement-related features [20]. |
Accessible Color Palettes (e.g., D3 schemeDark2) |
Pre-defined sets of colors that ensure sufficient contrast and are distinguishable to users with color vision deficiencies, improving chart clarity [26] [23]. |
| C. elegans Disease Models | Genetically modified worms (e.g., via CRISPR/Cas9) to carry mutations homologous to human diseases, providing a cost-effective in vivo model for screening [20]. |
| Functional Assays | Wet-lab experiments (e.g., enzyme inhibition, cell viability) that are essential for empirically validating the therapeutic activity predicted by AI models [24]. |
| Random Forest Classifier | A machine learning algorithm that is particularly effective for phenotypic data due to its ability to handle non-linear relationships and provide feature importance scores for interpretability [20]. |
Workflow & Pathway Diagrams
The High Cost of Irreproducible Results in Drug Discovery Timelines
Your Technical Support Center: Ensuring Reproducibility in HTS
This technical support center is designed to help researchers, scientists, and drug development professionals identify, troubleshoot, and prevent common issues that lead to irreproducible results in high-throughput screening (HTS). The following guides and FAQs are framed within the broader thesis that addressing reproducibility is critical for protecting the substantial investments in HTS campaigns, which involve large quantities of biological reagents, hundreds of thousands of compounds, and the utilization of expensive equipment [29].
Frequently Asked Questions (FAQs)
1. What are the most common sources of irreproducibility in an HTS workflow? Irreproducibility often stems from process-related errors rather than the biological question itself. Key areas to investigate include:
- Liquid Handling Inaccuracy: Improperly calibrated pipettes or dispensers can lead to inconsistent reagent or compound volumes across assay plates, causing significant well-to-well variation [29].
- Cell Line Instability: Using cells with high passage numbers or that are not properly authenticated can lead to genetic drift and changes in phenotypic response [29].
- Reagent Degradation: Improper storage or use of reagents beyond their stability period can reduce assay signal and increase background noise [29].
- Environmental Fluctuations: Uncontrolled factors like ambient temperature, CO₂ levels, and humidity during cell culture or assay incubation can alter results [3].
2. How can I quickly validate that my HTS process is reproducible before a full-scale screen? Before embarking on a full HTS campaign, it is essential to conduct a process validation. This involves:
- Running a Pilot Screen: Perform a smaller-scale screen using a representative subset of compounds and the complete planned workflow [29].
- Calculating Reproducibility Indexes: Use statistical measures to evaluate the results. For example, you can calculate the Z'-factor to assess the assay's robustness and signal-to-noise window. Other indexes, adapted from medical diagnostics, can be used to gauge the ability to distinguish active from non-active compounds reliably [29] [3].
3. Our negative controls are showing high signal, leading to a low signal-to-background ratio. What should I check? A high background signal in negative controls is a common troubleshooting issue. Follow this isolation process:
- Confirm Reagent Purity: Check for contamination in your buffer or media.
- Inspect Washing Steps: Ensure that aspiration/washing steps are thorough and consistent across all plates to remove unbound reagents.
- Check Substrate Specificity: Verify that your detection substrate (e.g., in a luciferase assay) is not reacting non-specifically.
- Test Individual Components: Systematically remove or replace individual assay components (e.g., the enzyme, substrate, or cell lysate) to identify the source of the background [30] [31].
4. We are seeing high well-to-well variation within the same assay plate. What is the likely cause? High intra-plate variation often points to a problem with liquid handling.
- Primary Cause: Check for clogged or poorly calibrated tips on your automated liquid handler. Perform a gravimetric analysis to check dispensing accuracy and precision.
- Secondary Cause: Ensure cells are evenly suspended and seeded at a consistent density across the entire plate. Aggregated cells can lead to uneven responses [29] [32].
5. A previously identified 'hit' compound fails to show activity in follow-up experiments. How should I investigate? This is a classic irreproducibility problem. Your investigation should focus on two areas:
- Compound Integrity: Re-test the original sample for purity and stability. Check for precipitation or degradation due to improper storage (e.g., repeated freeze-thaw cycles, exposure to light).
- Assay Conditions: Meticulously compare all experimental parameters between the original and follow-up experiments. Small differences in cell passage number, serum batch, incubation time, or reagent supplier can be the root cause [29] [3].
Troubleshooting Guides
Guide 1: Diagnosing a Failed HTS Pilot Screen
When a pilot screen fails to meet quality control standards (e.g., Z'-factor < 0.5), use this structured approach to diagnose the problem [30] [31].
Process:
Guide 2: Systematic Approach to Resolving Irreproducible Results Between Runs
For when you get conflicting results from the same experiment performed on different days [30] [31].
Process:
Experimental Protocols & Data Presentation
Key Reproducibility Metrics for HTS Process Validation
Before any full-scale screen, validate your process using these key metrics on a pilot run [29] [3].
| Metric | Calculation Formula | Target Value | Interpretation | ||
|---|---|---|---|---|---|
| Z'-Factor | `1 - [ (3σc⁺ + 3σc⁻) / | μc⁺ - μc⁻ | ]` | > 0.5 |
Measures the assay's robustness and quality. An excellent assay window. |
| Signal-to-Background (S/B) | μ_c⁺ / μ_c⁻ |
> 10 (or context-dependent) |
The ratio of positive control signal to negative control signal. | ||
| Signal-to-Noise (S/N) | (μ_c⁺ - μ_c⁻) / √(σ_c⁺² + σ_c⁻²) |
> 10 (or context-dependent) |
Indicates how well the signal can be distinguished from experimental noise. | ||
| Coefficient of Variation (CV) | (σ / μ) * 100% |
< 10-20% (depending on assay) |
Measures the dispersion of data points in a set of replicates. |
Protocol: HTS Process Validation
- Plate Design: Include at least 32 wells each of positive and negative controls on every 384-well assay plate. Distribute them evenly across the plate to monitor spatial bias [29].
- Pilot Run: Execute a screen of at least 3-5 plates using the full automation system and a small, diverse compound library (e.g., 1,000-5,000 compounds) [29].
- Data Analysis: Calculate the metrics in the table above for each plate. Any plate failing the Z'-factor target should be flagged, and the root cause investigated before proceeding [29] [3].
- Reproducibility Assessment: If possible, repeat the pilot run on a different day with a fresh preparation of key reagents. Compare the hit lists and potency rankings to assess inter-run reproducibility [3].
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and their functions for ensuring reproducible HTS experiments.
| Item | Function in HTS | Key Consideration for Reproducibility |
|---|---|---|
| Validated Cell Line | Biological system for phenotypic or target-based screening. | Use low passage stocks, regularly authenticate (e.g., STR profiling), and test for mycoplasma [29]. |
| Reference Agonist/Antagonist | Serves as the positive control for each assay plate. | Use a chemically stable compound with known, potent activity. Prepare fresh aliquots to avoid freeze-thaw cycles [29]. |
| Assay-Ready Plates | Source plates containing pre-dispensed compounds. | Ensure compound solubility and stability in DMSO over time. Store plates in sealed, humidity-controlled environments [29]. |
| Validated Antibody/Probe | Detection reagent for quantifying the assay signal. | Validate specificity and lot-to-lot consistency. Titrate to determine the optimal concentration for signal-to-background [29]. |
| Cell Viability Assay Kit | Counterscreen to rule out cytotoxic false positives. | Choose a kit that is non-toxic, homogenous, and compatible with your primary assay readout [32]. |
Implementing Robust HTS Workflows and Technologies
Strategic Assay Development and Plate Design to Minimize Systematic Error
Troubleshooting Guides
Guide 1: Troubleshooting Systematic Spatial Artifacts
Problem: Data shows unexplained patterns (e.g., edge effects, column-wise striping) that compromise reproducibility, even when traditional quality control metrics like Z'-factor appear acceptable.
Explanation: Spatial artifacts are systematic errors caused by uneven physical conditions across the assay plate. These can include evaporation gradients (edge effects), temperature fluctuations during incubation, or liquid handling inconsistencies. Traditional control-based metrics often fail to detect these issues because control wells only sample a limited portion of the plate [10].
Solution: Implement a dual-approach quality control strategy that combines traditional metrics with spatial artifact detection.
Step 1: Visual Inspection of Plate Heatmaps
- Generate a heatmap of the raw data from a control plate to visually identify patterns like strong edge effects or column/row striping.
- Protocol: Run a control plate with a uniform sample and create a heatmap where the color of each well represents its signal intensity. Patterns indicate systematic spatial artifacts.
Step 2: Apply Normalized Residual Fit Error (NRFE) Analysis
- Use the NRFE metric to quantitatively identify systematic errors in drug-treated wells that are missed by control-based metrics [10].
- Protocol: After fitting dose-response curves, calculate the NRFE. An NRFE value >15 indicates low-quality data that should be excluded or carefully reviewed. Values between 10-15 require additional scrutiny. This method is available through the
plateQCR package [10].
Step 3: Mitigate Identified Artifacts
- For edge effects, use specialized plate sealants or humidified incubators [33].
- For liquid handling errors, recalibrate instruments and ensure proper maintenance.
Guide 2: Addressing Poor Assay Robustness
Problem: The assay has a low Z'-factor or shows high variability between replicate plates, leading to an inability to distinguish true hits from background noise.
Explanation: Assay robustness is the ability to consistently detect a real biological signal. A low Z'-factor can stem from high variability in controls, a weak signal window, or temporal drift (degradation of reagents or instrument performance over time) [34] [33].
Solution: Optimize controls and validate assay performance over time.
Step 1: Select Appropriate Controls
- Use controls that reflect the strength of the hits you hope to find, not just the strongest possible effect. Consider using decreasing doses of a strong control to gauge sensitivity to realistic hits [34].
- Strategically place controls to minimize spatial bias; alternate positive and negative controls across available columns and rows instead of clustering them on the plate's edge [34].
Step 2: Perform Plate Drift Analysis
- This detects systematic temporal errors, such as reagent degradation or instrument warm-up effects, that can cause signals to drift from the first plate to the last in a screening run [33].
- Protocol: Run a series of identical control plates over the expected duration of your screening campaign. Plot the key performance metrics (e.g., Z'-factor, S/B) for each plate over time. A significant downward trend indicates plate drift.
Step 3: Optimize Replicate Strategy
- For complex phenotypes, more replicates (2-4) are often needed. The number is empirical and dictated by the signal-to-noise ratio of the biological response [34].
Guide 3: Preventing Sample Misidentification and Tracking Errors
Problem: Plates or samples are misidentified, leading to mixed-up data, lost tracks of specific plates, or misattributed results.
Explanation: In high-throughput environments, the sheer volume of plates processed increases the risk of human error, such as misreading handwritten labels or transposing data [35]. This is a pre-analytical error that can have severe consequences for data integrity.
Solution: Implement a robust, automated system for plate identification and tracking.
Step 1: Implement Barcode Labeling
- Label individual plates with barcodes that serve as a digital identifier, linking the plate to its experimental and sample data in your LIMS (Laboratory Information Management System) [35].
- For redundancy in automated workflows, apply barcodes to multiple sides of the microplate to ensure consistent identification regardless of orientation [35].
Step 2: Utilize Digital Well Plate Mapping
- Use a LIMS to digitally map individual wells, providing a comprehensive, interactive overview of the spatial arrangement of wells and associated experimental conditions [35].
Step 3: Establish Electronic Recordkeeping
- Replace paper notebooks and local spreadsheets with an Electronic Laboratory Notebook (ELN) or LIMS to centrally document experiment details, plate movements, and storage locations [35].
Frequently Asked Questions (FAQs)
Q1: What defines an acceptable Z'-factor for a high-throughput screening (HTS) assay? While a Z'-factor > 0.5 is a traditional cutoff for most HTS assays, a value in the range of 0 to 0.5 is often acceptable for complex phenotypic HCS (High-Content Screening) assays. These assays may yield more subtle but still biologically valuable hits. Good judgment should prevail, factoring in the complexity of the screen and the tolerance for false positives that can be filtered out later [34].
Q2: How many replicates are typically used in an HTS screen? Most large HTS screens are performed in duplicate. Increasing replicates from 2 to 3 represents a 50% increase in reagent cost, which is often prohibitive for screens involving tens of thousands of samples. The standard practice is to screen in duplicate and then retest hits in more robust confirmation assays with higher replicate numbers [34].
Q3: Why are control wells not sufficient for ensuring plate quality? Control-based metrics like Z'-factor are fundamentally limited because they only assess a fraction of the plate's spatial area. They cannot detect systematic errors that specifically affect drug wells, such as:
- Compound-specific issues (e.g., drug precipitation, assay interference).
- Spatial artifacts (e.g., evaporation gradients, pipetting errors) in regions not covered by controls [10].
Q4: How does plate miniaturization impact reagent cost and data variability? Miniaturization (e.g., moving from 384-well to 1536-well formats) significantly reduces reagent costs by decreasing the required assay volume. However, it amplifies data variability because volumetric errors become magnified in smaller volumes. This necessitates the use of extremely high-precision dispensers and strict control over evaporation [33].
Data Presentation
Table 1: Key Quality Control Metrics for HTS Assay Validation
| Metric | Formula/Description | Interpretation | Acceptable Range for HTS |
|---|---|---|---|
| Z'-factor [34] | 1 - [3(σ_p + σ_n) / |μ_p - μ_n|] |
Measures the separation band between positive (p) and negative (n) controls. Accounts for variability and dynamic range. | Ideal: >0.5, Acceptable for complex assays: 0 - 0.5 |
| Signal-to-Background (S/B) [33] | μ_p / μ_n |
The ratio of the mean signal of positive controls to the mean signal of negative controls. | >5 [10] |
| Strictly Standardized Mean Difference (SSMD) [10] | (μ_p - μ_n) / √(σ_p² + σ_n²) |
A robust measure for the difference between two groups that accounts for variability and is suitable for HTS. | >2 [10] |
| Normalized Residual Fit Error (NRFE) [10] | Based on deviations between observed and fitted dose-response values. | Detects systematic spatial artifacts in drug wells that are missed by control-based metrics. | Excellent: <10, Borderline: 10-15, Poor: >15 |
| Coefficient of Variation (CV) [33] | (σ / μ) * 100 |
Measures the dispersion of data points in a sample around the mean, expressed as a percentage. | Should be minimized; specific threshold depends on assay. |
Table 2: Common Systematic Errors and Mitigation Strategies
| Error Type | Common Causes | Impact on Data | Prevention Strategies |
|---|---|---|---|
| Edge Effects [34] | Uneven evaporation or heating from plate edges. | Over- or under-estimation of cellular responses in outer wells. | Use specialized plate sealants; humidified incubators; alternate control placement [34] [33]. |
| Liquid Handling Inaccuracies | Improperly calibrated or maintained dispensers. | Column/row-wise striping; high well-to-well variability. | Regular calibration; use of acoustic dispensers; verification with dye tests. |
| Plate Drift [33] | Reagent degradation, instrument warm-up, reader fatigue. | Signal window changes from the first to the last plate in a run. | Perform plate drift analysis during validation; use inter-plate controls. |
| Sample Mix-ups [35] | Human error in manual transcription; mislabeling. | Misattributed data; incorrect results linked to samples. | Implement barcode systems [35]; digital plate mapping [35]; two-person verification. |
Experimental Protocols
Protocol 1: Plate Drift Analysis for Temporal Stability
Purpose: To confirm that an assay's signal window and statistical performance remain stable over the entire duration of a large screening campaign [33].
Methodology:
- Preparation: Prepare a sufficient number of identical control plates containing positive and negative controls in their designated wells.
- Run Simulation: Over a period that mimics a full screening run (e.g., 8-24 hours), run these control plates through the entire automated HTS workflow at regular intervals.
- Data Collection: For each plate, calculate key performance metrics, including Z'-factor, S/B, and mean values for positive and negative controls.
- Analysis: Plot each metric against the time the plate was run. Visually and statistically analyze the plots for any significant trends (e.g., a linear decline in Z'-factor).
Protocol 2: NRFE Calculation for Spatial Artifact Detection
Purpose: To quantitatively identify systematic spatial errors in drug-treated wells that are not detected by traditional control-based QC methods [10].
Methodology:
- Data Prerequisite: Obtain a plate with dose-response data for multiple compounds.
- Curve Fitting: Fit a dose-response model (e.g., a 4-parameter logistic curve) to the data for each compound on the plate.
- Residual Calculation: For each well, calculate the residual—the difference between the observed response and the fitted value from the curve.
- Normalization: Normalize the residuals to account for the variance structure of dose-response data, applying a binomial scaling factor.
- NRFE Computation: Calculate the NRFE for the plate. Plates with an NRFE > 15 should be flagged for careful review or exclusion.
- Implementation: This protocol is implemented in the publicly available
plateQCR package (https://github.com/IanevskiAleksandr/plateQC) [10].
Workflow Visualization
Systematic Error Detection Workflow
Integrated Quality Control Strategy
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Strategic Assay Development |
|---|---|
| Barcoded Microplates [35] | Uniquely identifies each plate and links it to digital records, preventing misidentification and enabling seamless tracking through automated workflows. |
| Positive & Negative Controls [34] | Benchmarks for calculating assay quality metrics (e.g., Z'-factor). Should be selected to reflect the strength of expected hits, not just the strongest possible effect. |
| Electronic Laboratory Notebook (ELN)/LIMS [35] | Centralizes experimental data and metadata, enables digital well plate mapping, and ensures accurate, accessible, and complete electronic recordkeeping. |
| Plate Sealants & Humidified Incubators [33] | Mitigates edge effects by reducing evaporation gradients across the plate, a common source of spatial systematic error. |
| High-Precision Liquid Handlers | Ensures accurate and consistent dispensing of nanoliter volumes, critical for assay miniaturization and preventing systematic errors from pipetting inaccuracies. |
plateQC R Package [10] |
Provides a robust toolset for implementing the NRFE metric and other quality control analyses to detect spatial artifacts and improve data reliability. |
Leveraging Automation and Integrated Robotics for Reduced Human Variability
Technical Support Center
Frequently Asked Questions (FAQs)
What are the most common sources of human-induced variability in HTS, and how does automation address them? Human variability in HTS primarily arises from manual pipetting, inconsistencies in assay execution between users, and undocumented errors [4]. Automation addresses this through standardized robotic liquid handling, which ensures precise, sub-microliter dispensing identical across all wells and users [36] [37]. Integrated robotic systems also standardize incubation times and environmental conditions, eliminating these as sources of variation [36].
Our automated HTS runs are producing unexpected results. How do we determine if it's an assay or equipment issue? Begin by checking the quantitative metrics of your assay run. A sudden drop in the Z'-factor below 0.5 is a strong indicator of an assay quality or equipment performance issue [36] [38]. You should also:
- Inspect Control Values: Check if the mean values and coefficients of variation (CV) for your maximum and minimum control wells have deviated from established baselines. A high CV can point to liquid handling inconsistencies [38].
- Run a Diagnostic Test: Use the liquid handler's built-in verification features, if available. For example, technologies like DropDetection can verify that the correct volume was dispensed into each well [4].
- Check for Positional Effects: Create a heatmap of your readout signal across the microplate to identify patterns (like edge effects) that suggest environmental or washing inconsistencies [38].
We see patterns (e.g., row/column bias) in our HTS data heatmaps. What does this indicate? Positional effects, such as row or column biases, typically indicate technical issues related to the automated system rather than biological activity [38]. Common causes include:
- Liquid Handler Calibration: Improperly calibrated dispensers can lead to systematic volume errors across specific rows or columns.
- Plate Washer Performance: Inefficient washing can cause cross-contamination between adjacent wells.
- Incubator Conditions: A lack of uniform temperature or CO₂ across the plate can create gradients in cell-based assays. Investigate and service the specific module responsible for the pattern.
How can we ensure data integrity from our automated HTS platform for regulatory compliance? Robotics strengthen compliance by guaranteeing adherence to standardized procedures and robust reporting [39]. Implement a Laboratory Information Management System (LIMS) to track all experimental metadata, including compound identity, plate location, and instrument parameters, creating a full audit trail [36]. Furthermore, ensure your automated systems and data software are compliant with electronic records standards like 21 CFR Part 11 [36].
Our HTS workflow integrates instruments from different vendors. How can we prevent bottlenecks and failures? Integration of legacy instrumentation is a common challenge, often requiring custom middleware or protocol converters [36]. To mitigate this:
- Use a Central Scheduler: Employ orchestration software (e.g., FlowPilot) to manage timing and sequencing across all instruments [28].
- Prioritize API-enabled Instruments: When acquiring new equipment, select devices with modern Application Programming Interfaces (APIs) for flexible software control and easier integration [40] [28].
- Design for Failure Recovery: Choose robotic components with features like automated fault recovery and self-cleaning to minimize downtime [40].
Troubleshooting Guides
Problem: High Rate of False Positives/Negatives in Screening Campaign
| Potential Cause | Investigation Method | Corrective Action |
|---|---|---|
| Assay robustness is low | Calculate the Z'-factor for each assay plate. A score below 0.5 indicates a poor separation band between your controls [36]. | Re-optimize the assay protocol before proceeding with full-scale screening. This may involve adjusting reagent concentrations, incubation times, or cell seeding density. |
| Liquid handling inaccuracy | Use a photometric or gravimetric method to verify the volume dispensed by the liquid handler across the entire plate. | Re-calibrate the liquid handling instrument. For critical low-volume steps, consider using a non-contact dispenser to eliminate errors from tip wetting and adhesion [4]. |
| Undetected positional effects | Generate a heatmap of the primary readout (e.g., fluorescence intensity) for each plate to visualize row, column, or edge effects [38]. | Investigate and address the root cause, which may involve servicing the plate washer, validating incubator uniformity, or adjusting the liquid handler's method to pre-wet tips. |
| Inconsistent cell health | Use an automated cell counter (e.g., Accuris QuadCount) to ensure consistent viability and seeding density at the start of the assay [37]. | Standardize cell culture and passage procedures. Implement automated cell seeding to improve reproducibility across all assay plates. |
Problem: Low Z'-Factor on an Automated HTS Run
| Potential Cause | Investigation Method | Corrective Action |
|---|---|---|
| High variability in control wells | Check the Percent Coefficient of Variation (%CV) for both positive and maximum control wells. A CV >20% is a concern [38]. | Inspect the preparation of control solutions. Ensure the robotic method for dispensing controls is highly precise, potentially using a dedicated dispense step. |
| Poor signal-to-background (S/B) ratio | Calculate the S/B ratio. A ratio below a suitable threshold (e.g., 3:1) indicates a weak assay signal [38]. | Re-optimize assay detection parameters (e.g., gain, excitation/emission wavelengths) or consider using a more sensitive detection chemistry. |
| Instrument performance drift | Review the Z'-factor and control values by run date to identify a temporal trend, which may correlate with the last instrument service date [38]. | Perform full maintenance and calibration on the microplate reader and liquid handlers as per the manufacturer's schedule. |
Problem: Integration Failures in a Multi-Instrument Workcell
| Potential Cause | Investigation Method | Corrective Action |
|---|---|---|
| Communication failure between devices | Check the system scheduler log for error messages related to device time-outs or failed handshakes. | Verify physical connections and communication protocols (e.g., RS-232, Ethernet). Reset the connection and may require updating device drivers or the scheduler's communication middleware [36]. |
| Physical misalignment of robotic arm | Visually observe the robotic arm's movement during plate transfers to see if it accurately reaches deck positions. | Perform a re-homing sequence for the robotic arm and re-calibrate all deck positions according to the system's manual. |
| Inconsistent plate gripper operation | Run a diagnostic routine that tests the gripper's force and alignment. | Adjust the gripper force or replace worn gripper pads to ensure secure plate handling without jamming. |
Experimental Protocols for Validation and Troubleshooting
Protocol for Quantifying Assay Robustness (Z'-Factor Calculation)
Purpose: To quantitatively assess the quality and suitability of an assay for High-Throughput Screening by measuring the separation between positive and negative control populations [36] [38].
Materials:
- Assay reagents and cell line
- Positive control (known activator/inhibitor)
- Negative control (vehicle or buffer)
- Automated liquid handling system
- 384-well microplates
- Microplate reader
Methodology:
- Using the automated liquid handler, prepare at least 24 wells each of the positive control and negative control across multiple plates to capture inter-plate variability.
- Run the assay according to your standard protocol.
- On the microplate reader, measure the signal for all control wells.
- For each control population (positive and negative) on a plate, calculate:
- The mean of the signals (μpositive and μnegative)
- The standard deviation of the signals (σpositive and σnegative)
- Calculate the Z'-factor for the plate using the following equation [36]:
- Z' = 1 - [3(σpositive + σnegative) / |μpositive - μnegative|]
- Interpretation: A Z'-factor greater than 0.5 indicates an excellent assay robust enough for HTS. A Z'-factor between 0 and 0.5 may be usable but requires careful monitoring. A Z'-factor less than 0 indicates marginal or no separation between controls [36].
Protocol for Liquid Handler Performance Verification
Purpose: To validate the precision and accuracy of an automated liquid handling system, particularly for low-volume dispensing critical to miniaturized HTS [4] [37].
Materials:
- Automated liquid handler (e.g., I.DOT Non-Contact Dispenser, Accuris AutoMATE 96)
- A compatible, precise dye solution (e.g., tartrazine)
- UV-transparent 384-well microplate
- UV-Vis microplate reader
Methodology:
- Program the liquid handler to dispense the target volume (e.g., 1 µL) of the dye solution into every well of the microplate.
- Execute the dispense run.
- If the liquid handler is equipped with volume verification technology (e.g., DropDetection), review the log to confirm successful dispensing in all wells [4].
- Measure the absorbance of each well using the plate reader.
- Prepare a standard curve by dispensing and measuring known volumes/concentrations of the dye to correlate absorbance with volume.
- Analysis: Calculate the mean volume, standard deviation, and coefficient of variation (%CV) for all wells. A CV of less than 10% is generally acceptable, with lower values indicating higher precision. Compare the mean measured volume to the target volume to determine accuracy [37].
Table 1: Key Statistical Metrics for HTS Data Quality Assessment
| Metric | Calculation | Target Value | Significance | ||
|---|---|---|---|---|---|
| Z'-Factor | 1 - [3(σp + σn) / | μp - μn | ] | > 0.5 | Measures assay robustness and separation between positive (p) and negative (n) controls [36]. |
| Signal-to-Background (S/B) | μp / μn | > 3 | Indicates the strength of the assay signal relative to the background noise [38]. | ||
| Coefficient of Variation (CV) | (σ / μ) x 100 | < 20% | Measures the dispersion of data points in control wells; lower CV indicates higher precision [38]. | ||
| Signal-to-Noise (S/N) | (μp - μn) / √(σp² + σn²) | > 10 | Similar to S/B but incorporates variability; a higher value indicates a more reliable and detectable signal [38]. |
Table 2: Impact of Automation on Key HTS Parameters
| Parameter | Manual Process | Automated Process | Benefit of Automation |
|---|---|---|---|
| Throughput | ~100 samples/week [41] | >10,000 samples/day [41] | Dramatically accelerated screening timelines. |
| Liquid Handling Precision | High variability, especially at low volumes [4] | Sub-microliter accuracy with CV <10% [36] [37] | Improved data quality and reduced false positives/negatives. |
| Reproducibility | High inter- and intra-user variability [4] | Standardized workflows reduce variability [4] | Enables reproduction of results across users, sites, and time. |
| Operational Cost | High reagent consumption | Up to 90% reduction via miniaturization [4] | Significant cost savings per data point. |
Workflow and Process Diagrams
HTS Troubleshooting Logic
HTS System Validation Flow"
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Automated HTS
| Item | Function | Example Application |
|---|---|---|
| 384/1536-well Microplates | Miniaturized assay format that enables high-density screening and conserves expensive reagents [36]. | Standardized platform for all HTS assays. |
| Validated Control Compounds | Known active (positive) and inactive (negative) substances used to calibrate assays and calculate performance metrics like the Z'-factor [38]. | Assay validation and per-plate quality control. |
| Photometric Dye Solutions | Used in liquid handler performance verification to correlate absorbance with accurately dispensed volume [37]. | Periodic calibration of automated dispensers. |
| Cell Viability Assay Kits | Pre-optimized reagent kits (e.g., MTT, CellTiter-Glo) for measuring cell health and proliferation in automated cell-based screens. | Toxicity screening and normalization of cell-based data. |
| LIMS (Laboratory Information Management System) | Software platform that tracks all experimental metadata, ensures data integrity, and manages the audit trail for regulatory compliance [36]. | Centralized data management for all HTS projects. |
The Role of Advanced Liquid Handlers and Acoustic Dispensing in Precision
Technical Support Center: Troubleshooting Guides and FAQs
General Troubleshooting Guide
Q: My assay results show an unexpected pattern or trend. How do I determine if the liquid handler is the source? A: First, investigate if the pattern is repeatable. Run the test again to confirm the error is not a random event. A repeatable pattern often indicates a systematic liquid handling issue. Increasing the frequency of performance testing can help track the recurrence and pinpoint the root cause [42].
Q: What are the first steps I should take when I suspect a liquid handling error? A: Before assuming hardware failure, check the basics:
- Maintenance Schedule: Verify when the instrument was last serviced. Sedentary instruments are particularly prone to error [42].
- Liquid Class and Settings: Ensure the aspirate/dispense rates, heights, and liquid class settings are correctly defined for your specific reagent [43].
- Tip Quality and Fit: Always use vendor-approved tips. Cheap, low-quality tips can have variable wetting properties and may not fit correctly, leading to volume transfer errors [43].
Q: What are the economic impacts of liquid handling errors? A: Inaccurate liquid handling has direct and significant financial consequences:
- Over-dispensing expensive or rare reagents wastes precious materials. In a high-throughput lab screening millions of wells annually, a 20% over-dispense can cost over $750,000 per year [43].
- Under-dispensing can lead to an increase in false negatives, potentially causing a promising drug candidate to be overlooked, which could represent a loss of billions in future revenue [43].
Technology-Specific FAQs
Air Displacement Liquid Handlers
Q: What are common sources of error in air displacement systems? A: These systems are prone to errors caused by insufficient pressure or leaks in the air lines. A leaky piston or cylinder can cause a dripping tip and incorrect aspirated volumes. Regular maintenance of system pumps and fluid lines is essential [42].
Positive Displacement Liquid Handlers
Q: My positive displacement instrument is delivering volumes inaccurately. What should I check? A: Troubleshooting should include a thorough check of the fluidic path [42]:
- Ensure tubing is clean, clear, and free of kinks.
- Check for and remove any bubbles in the line.
- Verify there are no leaks and that all connections are tight.
- Ensure tubes are not too long or too short.
- Note that liquid temperature can affect flow rate and, thus, dispensing accuracy.
Acoustic Dispensing Systems
Q: My acoustic liquid handler (e.g., Labcyte Echo) is experiencing transfer inconsistencies or errors. What are the best practices? A: Acoustic dispensing requires specific preparation to function reliably [42] [44]:
- Thermal Equilibrium: Allow the source plate to equilibrate to room temperature before transfer.
- Centrifugation: Briefly centrifuge the source plate (e.g., 2 min at 1500 × g) before use to collect condensed fluid on the seal and level the well contents. This is imperative to avoid intermittent errors.
- Coupling Fluid: Regularly check the water coupling fluid system for air bubbles. Change the coupling media, clean filters, and purge the system if necessary.
- Calibration: Perform transducer focus calibrations regularly. Use the calibration setting designed for your specific sample composition (e.g., aqueous, DMSO, glycerol) to minimize error rates.
Q: Some commercial screening conditions fail to transfer acoustically. Why? A: Acoustic transfer compatibility depends on the physicochemical properties of the liquid. The table below summarizes the compatibility of various commercial screens with different acoustic instruments, highlighting that not all conditions are universally compatible [44].
Table 1: Acoustic Transfer Compatibility of Commercial Crystallization Screens
| Suite Name | Manufacturer | Labcyte Echo 550 Errors | Labcyte Echo 550 Success Rate | EDC ATS-100 Errors | EDC ATS-100 Success Rate |
|---|---|---|---|---|---|
| Crystal Screen HT | Hampton Research | 0 | 100% | -- | -- |
| PEG/Ion HT | Hampton Research | 0 | 100% | -- | -- |
| Index HT | Hampton Research | 1 | 99% | 8 | 92% |
| Morpheus | Molecular Dimensions | 0 | 100% | -- | -- |
| MIDASplus | Molecular Dimensions | 19 | 80% | -- | -- |
| Wizard I & II | Emerald Biosciences | 0 | 100% | 7 | 93% |
| JCSG+ | Nextal | -- | -- | 11 | 89% |
Q: How do calibration settings affect performance on a Labcyte Echo system? A: The choice of instrument calibration directly impacts transfer speed and error rate. Using a calibration designed for your specific plate type and liquid composition is critical for optimal performance [44].
Table 2: Impact of Calibration Settings on a Labcyte Echo 550
| Calibration Setting | Designed For | Transfer Time | Error Rate |
|---|---|---|---|
| 384PPAQCP | Aqueous Crystallization Conditions | 59 s | 0% |
| 384PPAQSP2 | Aqueous Solutions | 29 s | 3.1% |
| 384PP_DMSO2 | DMSO | 34 s | 7.3% |
| 384PPAQBP2 | Glycerol-based Solutions | 30 s | 5.2% |
| 384PPAQGP2 | Glycerol-based Solutions | 26 s | 21.9% |
Common Error Reference Table
The following table lists frequently observed errors, their possible sources, and recommended solutions.
Table 3: Common Liquid Handling Errors and Solutions
| Observed Error | Possible Source of Error | Possible Solutions |
|---|---|---|
| Dripping tip or drop hanging from tip | Difference in vapor pressure of sample vs. water; Leaky piston/cylinder | Sufficiently prewet tips; Add air gap after aspirate; Regular maintenance [42] |
| Droplets or trailing liquid during delivery | Viscosity and other liquid characteristics different than water | Adjust aspirate/dispense speed; Add air gaps or blow outs [42] |
| Diluted liquid with each successive transfer | System liquid is in contact with sample | Adjust leading air gap [42] |
| First/last dispense volume difference | Sequential dispense method | Dispense first/last quantity into a reservoir or waste [42] |
| Serial dilution volumes varying from expected concentration | Insufficient mixing | Measure and improve liquid mixing efficiency [42] [43] |
| Intermittent transfer failures (Acoustic) | Air bubbles in coupling fluid; Condensed fluid on source plate seal | Purge coupling fluid system; Centrifuge source plate before use [44] |
Detailed Experimental Protocol: Acoustic Dispensing for Crystallization Screens
This protocol, adapted for a Labcyte Echo system, ensures precise nanoliter-scale dispensing for setting up crystallization trials [44].
Workflow: Acoustic Dispensing for Crystallization Trials
Materials and Reagent Solutions
- Acoustic Dispensing System: e.g., Labcyte Echo 550 or 650 [44] [45].
- Source Plate: 384-well polypropylene Echo Qualified plate (e.g., Labcyte PP-0200) or Low Dead Volume plate for precious samples [44].
- Destination Plate: Sitting drop crystallization plate (e.g., Swissci 96-well 3-drop low profile plate). Ensure the plate flange is compatible with the instrument's locking mechanism [44].
- Coupling Fluid: Deionized, degassed water. Must be free of bubbles to prevent acoustic interference [44] [45].
- Sealing Foil: Optically clear, sealable foil (e.g., Greiner EASYseal film) [44].
Step-by-Step Methodology
- Preparative Work:
- Prepare the source plate with your crystallization conditions, sealing it if not used immediately.
- In the instrument software, define the geometry of your specific destination plate. This may require setting manual offsets for irregular plate layouts [44].
- Prepare a separate deep-well block with screen conditions for reservoir dispensing, as acoustically dispensing large reservoir volumes is not efficient [44].
System Preparation:
- Equilibrate the prepared source plate to room temperature [44].
- Crucially, centrifuge the sealed source plate briefly (2 minutes at 1500 × g) to collect any condensed fluid on the seal and level the liquid in the wells. This step is vital for transfer consistency [44].
- In the instrument software, set up the transfer protocols. Use a calibration designed for aqueous crystallization conditions (e.g.,
384PP_AQ_CP) for the lowest error rate, even if transfer times are longer. Protein samples can often be transferred with faster calibrations (e.g.,384PP_AQ_BP2) [44]. - Check the coupling fluid system thoroughly for air bubbles and purge if necessary. Perform a transducer focus calibration [44].
Acoustic Transfer:
- The instrument will first perform an acoustic audit of the source plate, using low-energy sound pulses to determine the fluid level and acoustic properties in each well [45].
- Execute the transfer protocol to dispense screen conditions into the destination plate. For a 1:1 protein-to-condition ratio, a final drop size of at least 50 nL is recommended to prevent premature drying [44].
- Immediately after the plate is ejected, cover it with a glass or plastic sheet to limit evaporation.
- Transfer the protein solution to the condition drops using the established protocol.
Post-Dispensing:
- Fill the reservoir wells of the destination plate with solution from the deep-well block (e.g., 30 μL per reservoir) using a multichannel pipette [44].
- Seal the destination plate completely using microplate sealing foil.
The Researcher's Toolkit: Essential Materials for Acoustic Dispensing
Table 4: Key Reagent Solutions and Materials
| Item | Function | Key Consideration |
|---|---|---|
| Echo-Qualified Source Plates | Holds samples for acoustic ejection. | Polypropylene (PP-0200) for general use; Low Dead Volume (LP-0200) for precious samples [44]. |
| Coupling Fluid | Interface between transducer and plate bottom to transmit sound waves. | Must be degassed and free of bubbles to prevent signal disruption [45]. |
| Sealing Foils | Seals source and destination plates to prevent evaporation and contamination. | Ensure compatibility with storage conditions and downstream analysis (e.g., UV-transparency) [44]. |
| Instrument Calibrations | Pre-set parameters for specific liquid and plate types. | Selecting the correct calibration (e.g., for aqueous, DMSO, or glycerol solutions) is critical for accuracy and low error rates [44]. |
In high-throughput screening (HTS), the integrity and quality of compound libraries are foundational to research reproducibility. Compound-mediated assay interference is a major contributor to false-positive results and irreproducible findings in early drug discovery [46] [47]. Establishing rigorous protocols for library storage and quality control (QC) is therefore not merely a logistical concern but a critical scientific imperative for generating reliable, actionable data.
This guide provides troubleshooting and best practices to help researchers maintain compound integrity, thereby enhancing the validity of their HTS outcomes.
Compound Storage: Conditions and Stability
Proper storage conditions are the first line of defense against compound degradation. The following table summarizes key parameters and their specifications.
| Storage Parameter | Recommended Specification | Impact on Compound Integrity |
|---|---|---|
| Temperature | -20°C or lower (e.g., -80°C for long-term) | Prevents chemical decomposition and maintains compound stability [46] |
| Solvent | DMSO (100% or at high concentration) | Serves as a standard cryoprotectant solvent for library storage [46] |
| Freeze-Thaw Cycles | Minimized (e.g., single-use aliquots) | Repeated freezing and thawing in DMSO introduces water, leading to hydrolysis and precipitation [46] |
| Humidity Control | Low-humidity environment | Prevents water absorption from the atmosphere, which can cause hydrolysis and microbial growth [46] |
Quality Control and Hit Validation Methodologies
After establishing a robust storage protocol, the next step is implementing a cascade of experimental QC strategies to triage primary hits and eliminate artifacts [47]. The table below details key experimental approaches.
| Methodology | Primary Function | Key Techniques & Reagents |
|---|---|---|
| Dose-Response Confirmation | Confirm activity and determine potency (IC50) | Generate dose-response curves; steep or bell-shaped curves may indicate toxicity or aggregation [47] |
| Counter Screens | Identify and eliminate false-positive hits from assay technology interference | Assays using same detection technology without biological target; add BSA or detergents to counter aggregation [47] |
| Orthogonal Assays | Confirm bioactivity using an independent readout technology | Use luminescence or absorbance if primary was fluorescence; SPR, ITC, MST for binding validation [47] |
| Cellular Fitness Assays | Exclude generally cytotoxic compounds | Cell viability (CellTiter-Glo, MTT), cytotoxicity (LDH assay, CytoTox-Glo), apoptosis (caspase assay) [47] |
Troubleshooting FAQs
Q1: A significant portion of our hit compounds show activity in the primary screen but fail in concentration-response. What could be the cause?
This is often due to compound precipitation or chemical instability. Ensure compounds are stored in a dry, cold environment with minimal freeze-thaw cycles. During screening, use freshly thawed aliquots and consider adding low concentrations of detergents like Triton X-100 to the assay buffer to disrupt compound aggregates [46] [47]. Also, inspect the shape of the dose-response curves; shallow or irregular curves can indicate poor compound behavior.
Q2: Our cell-based HTS yielded many hits that turned out to be fluorescent or cytotoxic. How can we flag these earlier?
Implement targeted counter and cellular fitness screens as part of your standard triage cascade [47].
- For fluorescent compounds, run the compounds in the assay buffer without the detection reagents.
- For cytotoxicity, run a parallel viability assay (e.g., CellTiter-Glo) on the cell line used in the primary screen. Hits that reduce cell viability in this counter-screen are likely non-specific cytotoxins and should be deprioritized.
Q3: How can we be more confident that a hit is truly engaging the biological target?
Incorporate orthogonal and biophysical assays into the validation workflow. An orthogonal assay that measures the same biology but with a different readout (e.g., switching from fluorescence to luminescence) can rule out technology-specific interference. For target-based screens, techniques like Surface Plasmon Resonance (SPR) or thermal shift assays can provide direct evidence of target binding and help prioritize hits with the highest confidence [47].
Experimental Protocol: Hit Triage Cascade
This protocol outlines a sequential approach to validate hits from a primary screen, integrating counter, orthogonal, and cellular fitness assays to prioritize high-quality leads [47].
Workflow Overview:
Procedure:
- Primary Screening: Conduct your HTS or HCS campaign under optimized and robust assay conditions. Identify the initial set of "primary hits" based on the chosen activity threshold [47].
- Dose-Response Confirmation:
- Re-test the primary hits in a concentration-dependent manner (e.g., a 10-point, 1:3 serial dilution).
- Calculate IC50/EC50 values. Discard compounds that do not show a reproducible dose-response relationship.
- Note: The curve shape is informative. Steep curves may suggest aggregation, while bell-shaped curves can indicate cytotoxicity at higher concentrations [47].
- Counter Screens:
- Design assays that mimic the primary screen's detection technology but lack the key biological component (e.g., the enzyme in a biochemical assay).
- Compounds that show "activity" in this counter-screen are likely interfering with the assay technology (e.g., by fluorescing or quenching the signal) and should be removed from consideration [47].
- Orthogonal Assays:
- Re-test the remaining hits using an assay that measures the same biological outcome but employs a fundamentally different detection method (e.g., switch from fluorescence to luminescence or a biophysical method like SPR) [47].
- This step confirms that the observed biological effect is genuine and not an artifact of the initial readout.
- Cellular Fitness Screens:
- Subject the validated hits to cellular health assays to rule out general toxicity.
- Use bulk-readout assays like CellTiter-Glo (viability) or CytoTox-Glo (cytotoxicity). For a more detailed morphological profile, employ high-content imaging with stains for nuclei, mitochondria, and membrane integrity (e.g., "cell painting" assay) [47].
- Deprioritize compounds that show significant toxicity at or near their active concentration.
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and solutions used in the featured hit triage experiments.
| Reagent / Solution | Function in Experiment |
|---|---|
| DMSO (100%) | Standard cryoprotectant solvent for compound library storage; prevents ice crystal formation [46] |
| BSA or Detergents (e.g., Triton X-100) | Added to assay buffers to reduce nonspecific compound binding and prevent aggregation-based false positives [47] |
| CellTiter-Glo / MTT Reagent | Measures cellular ATP levels/metabolic activity as a standard indicator of cell viability in cellular fitness screens [47] |
| LDH Assay Reagents | Quantifies lactate dehydrogenase release from damaged cells, a marker of cytotoxicity [47] |
| High-Content Staining Dyes (DAPI, MitoTracker) | Fluorescent dyes for multiplexed imaging of cellular structures (nuclei, mitochondria) to assess compound-induced morphological changes and toxicity [47] |
Technical Support Center
This technical support center addresses common informatics challenges that impact data fidelity and reproducibility in High-Throughput Screening (HTS). Ensuring seamless compound tracking and robust data analysis is crucial for generating reliable, reproducible results in drug discovery [48] [3]. The guidance below provides solutions to specific technical issues researchers may encounter during their experiments.
Troubleshooting Guides
Issue 1: Inconsistent Compound Location Tracking in HTS Workflow
Problem: Users report difficulties in accurately tracking the physical location and usage of compound source plates during screening campaigns, leading to potential sample misidentification.
Investigation Steps:
- Verify the integration between the sample management software (e.g., Titian Mosaic SampleBank) and the automated storage system (e.g., HighRes) [48].
- Check the continuous feedback logging from the storage system to the sample management database for errors or interruptions [48].
- Confirm that all assay plates are correctly barcoded and that these barcodes are successfully uploaded and linked to sample ID and location data in the informatics platform [48].
Resolution:
- Restore the feedback loop between the HighRes system and Mosaic software. A system reboot may be necessary.
- Manually validate a subset of plate barcodes against the database to ensure data fidelity.
- If the issue persists, inspect the library source plates for damage or misplacement within the automated store and re-scan them [48].
Issue 2: Low Data Correlation Between Screening Replicates
Problem: Primary screening data shows low correlation between experimental replicates, raising concerns about reproducibility and the ability to distinguish true active compounds [6] [3].
Investigation Steps:
- Assess the assay's validation data, specifically the Z'-factor from the pilot screen, to confirm robust assay performance [48] [49].
- Review the raw data for a high incidence of missing values (e.g., dropouts in signal) which can skew correlation measures if not handled properly [6].
- In your data analysis software (e.g., Genedata Screener), check the normalization and correction methods applied to the raw data [48].
Resolution:
- If the Z'-factor is below 0.5, re-optimize the assay conditions before proceeding.
- For datasets with a large number of missing values, employ statistical methods designed to account for them, such as correspondence curve regression (CCR) with a latent variable approach, rather than simply excluding missing data points [6].
- Apply appropriate background correction and normalization protocols to the raw intensity data to remove technical noise [48] [3].
Issue 3: Failed Quality Control (QC) for Hit Potency Assessment
Problem: Compounds advancing to the hit validation phase fail QC checks during potency determination (e.g., EC/IC50), indicating potential compound degradation or miscalculation.
Investigation Steps:
- Check the QC history of the specific HTS library source plate via the integrated informatics platform [48].
- Verify the LCMS analysis results for the failed compounds to confirm identity and purity [48] [49].
- Review the acoustic dispensing (e.g., Echo) logs for the assay plate in question to ensure accurate compound transfer [48].
Resolution:
- Re-source the compound from freshly stocked solids and repeat the potency assay.
- If the issue is widespread, perform a broader QC check on the library source plates stored in the automated compound store.
- Recalibrate the acoustic dispenser to ensure precise compound delivery in the nanoliter range [48].
Issue 4: inability to Compare Chromatography Data Across Vendors
Problem: Researchers cannot seamlessly compare chromatography results and methods from different CDS vendors, instruments, or sites, hindering data integration for R&D.
Investigation Steps:
- Confirm the data format of the source files. The platform may require specific data formats for successful integration [50].
- Verify that the metadata mapping for each vendor's system has been correctly configured for your organization's needs [50].
Resolution:
- Use a platform that automatically transforms chromatography data into a vendor-neutral, standardized format (e.g., Allotrope Foundation's .ASM) upon ingestion [50].
- Utilize a universal chromatography viewer within the platform to overlay and compare chromatograms and peak information from different sources directly [50].
Frequently Asked Questions (FAQs)
Q1: What are the best practices for maintaining compound integrity in our HTS library? A dedicated, custom-built storage facility with controlled low humidity and ambient temperature is essential. Furthermore, implement regular quality control (QC) checks using Liquid Chromatography-Mass Spectrometry (LCMS) on library source plates and maintain a fully integrated informatics platform for precise compound tracking and management [48] [49].
Q2: How can we improve the reproducibility of our HTS workflow when many measurements are missing? Traditional reproducibility measures like correlation can be misleading with missing data. Implement advanced statistical methods like correspondence curve regression (CCR) that use a latent variable approach to incorporate missing values into the reproducibility assessment, providing a more accurate picture of your workflow's performance [6].
Q3: Our hit confirmation rates are low. What could be the cause? Low hit confirmation rates often stem from assay artifacts or compound interference. In addition to rigorous assay development, incorporate targeted counter-screens and orthogonal assays early in the hit triage process. A flexible informatics platform that allows for nuanced hit selection strategies helps balance the reduction of false positives with the risk of excluding false negatives [48] [49].
Q4: How can we ensure data fidelity from the assay plate through to the final analysis? A robust informatics strategy is key. This includes using barcoded assay plates, whose data is uploaded to an analysis platform like Genedata Screener. The integration of plate barcodes with sample ID and location data from the compound management system (e.g., Mosaic) guarantees data fidelity throughout the process and enables detailed analysis by plate, batch, and screen [48].
Q5: What should we look for in an informatics platform to support reproducible HTS? The platform should offer:
- Integrated compound management for tracking source plates and assay plates [48].
- Seamless data integration that links sample identity with screening results [48].
- Advanced data analysis capabilities to handle large, complex datasets and facilitate reproducibility analysis [48] [6].
- Vendor-neutral data transformation to enable comparison of data from different instruments and sites [50].
Key Experimental Protocols and Data
Protocol: Assessing HTS Reproducibility with Missing Data
This protocol uses an extension of Correspondence Curve Regression (CCR) to properly account for missing values, which are common in single-cell RNA-seq and other HTS experiments [6].
- Data Collection: For each workflow being compared, collect significance scores (e.g., p-values, expression levels) for a list of candidates (e.g., genes) from two or more replicate experiments.
- Handle Missingness: Assume that unobserved candidates (e.g., dropouts) received a score lower than all observed candidates. Candidates observed in at least one replicate are "partially observed."
- Model Specification: The model assesses the probability that a candidate consistently passes rank-based selection thresholds in different replicates. It uses a cumulative link model to summarize the effects of operational factors (e.g., platform, sequencing depth) on reproducibility as regression coefficients.
- Estimation: Use a latent variable approach to incorporate information from partially observed candidates, allowing for a principled assessment of how operational factors affect reproducibility even with substantial missing data [6].
Quantitative Reproducibility Data
The table below summarizes how different reproducibility measures can lead to conflicting conclusions when applied to the same single-cell RNA-seq data, highlighting the need for specialized methods.
| Library Preparation Kit | Spearman Correlation (All Data) | Spearman Correlation (Non-Zero Data Only) | Pearson Correlation (All Data) | Pearson Correlation (Non-Zero Data Only) |
|---|---|---|---|---|
| TransPlex | 0.648 | 0.501 | More reproducible | More reproducible |
| SMARTer Ultra Low | 0.734 | 0.460 | Less reproducible | Less reproducible |
Source: Adapted from analysis of HCT116 cells single-cell RNA-seq data [6].
Workflow and Pathway Visualizations
HTS Informatics and Data Analysis Workflow
The diagram below outlines the key stages of a robust HTS informatics workflow, from compound storage to final hit identification, emphasizing points of integration critical for data fidelity.
Data Analysis and Reproducibility Assessment Pathway
This pathway illustrates the logical flow for analyzing HTS data and assessing reproducibility, particularly when dealing with missing values.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item | Function in HTS |
|---|---|
| LeadFinder Diversity Library | An extensive collection of 150,000 compounds with low molecular weight and lead-like properties, designed to provide high-quality starting points for drug discovery projects [48] [49]. |
| Prism Library | A drug-like compound library with high chirality and FSP3, featuring novel natural product-inspired scaffolds. Offers enhanced intellectual property protection by excluding hit structures from subsequent screens for two years [48] [49]. |
| Focused Libraries (e.g., PPI, Kinase) | Specialized sets, such as the Enamine Protein-Protein Interaction library, which contain compounds designed to target specific biological mechanisms or protein families [48] [49]. |
| LCMS (Liquid Chromatography-Mass Spectrometry) | A critical quality control tool used to meticulously analyze samples from HTS library source plates to verify compound identity and purity, ensuring data reliability [48] [49]. |
| Acoustic Dispenser (e.g., Echo) | Provides highly accurate, non-contact transfer of compounds in the nanoliter range, which is essential for minimizing volumes and ensuring precision in assay setup [48]. |
Troubleshooting Common HTS Pitfalls and Optimizing Performance
High-throughput screening (HTS) assays are pivotal in modern biomedical research, enabling the rapid evaluation of vast libraries of compounds or biological entities in fields like drug discovery and functional genomics [51]. Ensuring the quality and reliability of HTS data is critical, as technical variability from factors like plate-to-plate differences or reagent inconsistencies can compromise data integrity, leading to erroneous conclusions and wasted resources [51]. Statistical metrics for quality control (QC) assess an assay's performance in distinguishing between positive and negative controls, which is fundamental for establishing confidence in measurements and evaluating workflow performance [6] [51].
The Z-factor was one of the earliest adopted QC metrics, providing a simple measure of assay quality by accounting for variabilities in both positive and negative controls [52]. However, its absolute value and mathematical inconvenience for deriving statistical inference limited its interpretability [52]. The Strictly Standardized Mean Difference (SSMD) was subsequently proposed as a robust alternative, offering a probabilistic basis, better interpretability, and a more reliable approach for assessing effect sizes and assay quality [52] [51].
This guide addresses common challenges and questions researchers face when implementing these QC metrics, particularly in the context of addressing reproducibility issues in HTS research. We provide troubleshooting advice, practical protocols, and comparisons to help you select and apply the most appropriate metric for your experiments.
Troubleshooting Guides & FAQs
FAQ 1: What are the key limitations of the Z-factor that led to the development of SSMD?
While the Z-factor was a valuable initial QC metric, several critical limitations affected its utility and reliability:
- Limited Interpretability: The absolute sign in the Z-factor formula makes it mathematically inconvenient to derive its statistical inference [52].
- Inadequate for Moderate Controls: The Z-factor-based QC criterion is most suitable for assays with very or extremely strong positive controls. In RNAi HTS assays, a strong or moderate positive control is often more instructive, as its effectiveness is more similar to the hits of interest. The Z-factor performs poorly in these common scenarios [52].
- Inconsistent Results for Multiple Controls: It is common practice to adopt two or more positive controls in a single experiment. Applying Z-factor-based QC criteria to different types of controls (e.g., moderate vs. strong) within the same experiment can lead to inconsistent and misleading results [52].
SSMD was developed to overcome these issues by providing a metric with a strong probabilistic basis, direct interpretability through its link with d⁺-probability, and reliable performance across different types of controls and effect sizes [52] [51].
FAQ 2: How does SSMD provide a better measure of effect size and quality control compared to the Z-factor?
SSMD offers a more nuanced and statistically sound approach to QC for several reasons:
- Probabilistic Foundation: SSMD has a strong link with d⁺-probability (the probability that the difference between two groups is positive). This makes its interpretation more intuitive [52] [51].
- No Built-in Absolute Value: Unlike the Z-factor, SSMD is not defined with an absolute value, which facilitates easier mathematical derivation of its statistical inferences, such as confidence intervals [52].
- Comprehensive Quality Assessment: SSMD directly measures the magnitude of difference between two groups. For HTS assays that are preprocessed using log-transformation, SSMD represents the mean of log fold change divided by its standard deviation. In essence, it is the average fold change (on the log scale) penalized by its variability, providing a more integrated view of assay performance [52].
- Established Quality Thresholds: SSMD provides clear, tiered thresholds for classifying assay quality based on the strength of the positive control, leading to more consistent and informative QC assessments [52].
Table 1: SSMD-based QC Criteria for Classification of Assay Quality
| Quality Type | Moderate Control | Strong Control | Very Strong Control | Extremely Strong Control |
|---|---|---|---|---|
| Excellent | β ≤ -2 | β ≤ -3 | β ≤ -5 | β ≤ -7 |
| Good | -2 < β ≤ -1 | -3 < β ≤ -2 | -5 < β ≤ -3 | -7 < β ≤ -5 |
| Inadequate | β > -1 | β > -2 | β > -3 | β > -5 |
FAQ 3: When should I use SSMD versus AUROC (Area Under the ROC Curve) for quality control?
SSMD and AUROC are complementary metrics that together provide a comprehensive evaluation of assay performance.
- SSMD is a standardized measure of effect size. It quantifies the separation between positive and negative controls, accounting for their variability. It is prized for its interpretability and established QC thresholds [51].
- AUROC provides a threshold-independent assessment of discriminative power. It represents the probability that a randomly selected positive control will be ranked higher than a randomly selected negative control and is equivalent to the d⁺-probability [51].
You should use both for a robust QC practice. SSMD helps you understand the size of the effect you are trying to detect, while AUROC evaluates the assay's inherent ability to classify hits correctly across all possible thresholds. Their relationship is well-defined under certain distributional assumptions, such as AUROC = Φ(SSMD) for normal distributions, where Φ is the standard normal cumulative distribution function [51].
FAQ 4: How should I handle missing data or a high number of zero counts in my reproducibility assessment?
In high-throughput experiments like single-cell RNA-seq, a majority of reported expression levels can be zero due to dropouts, creating many missing observations [6]. A common but flawed practice is to exclude these missing values from reproducibility assessments.
- The Problem: Excluding missing values can generate misleading assessments. If only a small proportion of non-zero measurements agree well but the rest are observed only on a single replicate, ignoring zeros can suggest high reproducibility despite widespread discordance [6].
- The Solution: Use statistical methods designed to incorporate missing values. For instance, an extension of Correspondence Curve Regression (CCR) uses a latent variable approach to include candidates with unobserved measurements. This principled approach prevents biased assessments by properly accounting for the information contained in missing data patterns [6].
FAQ 5: What is the practical workflow for applying a QbD framework to my preclinical assay development?
Quality by Design (QbD) is a systematic framework for building quality into your assay from the beginning. The following workflow, illustrated in the diagram below, outlines the key steps:
Title: QbD Workflow for Preclinical Assay Development
- Scoping Phase: Begin with a clear definition of the assay's objectives and a plan for downstream validation. This involves reviewing literature and prior knowledge [53].
- Define Critical Quality Attributes (CQAs): These are the characteristics that define your desired assay quality. Common CQAs include:
- Identify Critical Process Parameters (CPPs): These are the assay variables (e.g., incubation time, reagent concentration) known to affect the CQAs [53].
- Design of Experiments (DoE): Use statistical DoE to systematically and efficiently investigate the relationship between CPPs and CQAs. This is more efficient than testing one factor at a time [53].
- Run Experiment and Analyze Data: Execute your designed experiment and analyze the data to model how CPPs affect CQAs.
- Define the Design Space: This is the multidimensional combination of CPP levels that will result in acceptable CQA values. Operating within this space ensures assay robustness against small, inadvertent changes in protocol [53].
Experimental Protocols
Protocol 1: Estimating SSMD for Quality Control
This protocol details the methods for estimating SSMD in an HTS QC setting, such as when comparing positive and negative controls on an assay plate.
1. Materials and Reagents Table 2: Key Research Reagent Solutions for HTS QC
| Item | Function / Description |
|---|---|
| Positive Control | A compound or sample with a known, reproducible effect that establishes the upper response limit of the assay. |
| Negative Control | A compound or sample with no expected effect (e.g., vehicle control) that establishes the baseline or lower response limit. |
| Assay Plates | Multi-well plates (e.g., 384-well or 1536-well) formatted with positive and negative controls. |
| Reagents for Detection | Components required to generate a measurable signal (e.g., luminescent, fluorescent). |
2. Procedure
- Experimental Design: Plate your positive and negative controls. The number of wells for each control (nP and nN) should be reasonably large, a common feature in 384-well or 1536-well platforms [52].
- Data Collection: Run your HTS assay and collect the measured values (e.g., fluorescence intensity) for all control wells.
- Choose an Estimation Method: The choice of estimator depends on your data and the goal.
- For robust estimation without outliers: Use the method-of-moment (MM) estimate.
- Calculate the sample means (X̄P, X̄N) and standard deviations (sP, sN) for the positive and negative controls.
- Apply the formula: β̂ = (X̄P - X̄N) / √(sP² + sN²) [52].
- For data with clearly present outliers: Use a robust estimate.
- Calculate the medians (X̃P, X̃N) and median absolute deviations (s̃P, s̃N) for the two groups.
- Apply the formula: β̂ = (X̃P - X̃N) / (1.4826 * √(s̃P² + s̃N²)) [52].
- For higher accuracy with normal data and equal variance: Use the uniformly minimum variance unbiased estimate (UMVUE).
- Calculate the sample means and the pooled variance.
- Apply the formula: β̂ = (X̄P - X̄N) / √( (2/K) * ( (nP-1)sP² + (nN-1)sN² ) ), where K ≈ nP + nN - 3.48 [52].
- For robust estimation without outliers: Use the method-of-moment (MM) estimate.
3. Data Analysis
- Calculate your chosen SSMD estimate from the collected data.
- Refer to the SSMD-based QC criteria (Table 1) to classify your assay quality as "Excellent," "Good," or "Inadequate" based on the strength of your positive control.
Protocol 2: Integrating SSMD and AUROC for Comprehensive QC
This protocol outlines how to jointly use SSMD and AUROC to get a complete picture of your assay's performance.
1. Procedure
- Calculate SSMD: Follow Protocol 1 to obtain an SSMD estimate for your control data.
- Calculate AUROC: Use a non-parametric method for broad applicability.
- Use the Mann-Whitney U Statistic [51]. This involves:
- Ranking all measured values from both positive and negative controls together.
- Calculating the U statistic: U = nP * nN + (nP(nP+1))/2 - RP, where RP is the sum of the ranks of the positive controls.
- Then, AUROC = U / (nP * nN).
- Alternatively, use established statistical software (e.g., the
pROCpackage in R orscikit-learnin Python) which can compute this efficiently and also provide confidence intervals via methods like DeLong's or bootstrapping [51].
- Use the Mann-Whitney U Statistic [51]. This involves:
2. Data Analysis
- Interpret SSMD: Check if the SSMD value meets the desired threshold for your assay quality (see Table 1).
- Interpret AUROC:
- AUROC = 1: Perfect discrimination.
- AUROC = 0.5: No discriminative power (random guessing).
- AUROC < 0.5: Inverted classification.
- Check Consistency: For normally distributed data, you can verify the internal consistency of your metrics by checking if AUROC ≈ Φ(SSMD). Large discrepancies may indicate violations of distributional assumptions or outliers, prompting a review of your data or a switch to more robust estimation methods [51].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for HTS QC and Reproducibility Analysis
| Item / Solution | Function in the Experiment |
|---|---|
| Positive Control Compounds | Provides a known strong signal to define the upper dynamic range and calculate metrics like SSMD and Z-factor. |
| Negative Control (Vehicle) | Establishes the baseline signal and is critical for defining the noise level in the assay. |
| Reference Standards | Well-characterized materials used to calibrate assays and monitor performance across multiple experimental runs. |
| Cell Lines with Known Genetic Modifications | Used in cell-based assays (e.g., CRISPR screens) as biologically relevant positive and negative controls [53]. |
| Detection Reagents (Luminescent/Fluorescent) | Enzymes, substrates, or dyes that generate a measurable signal proportional to the activity or concentration of the target. |
| Statistical Software (R, Python, JMP) | Essential for calculating QC metrics (SSMD, AUROC), performing DoE, and defining the design space [53] [51]. |
Troubleshooting Guides & FAQs
FAQ: Fundamental Concepts
Why is temperature management so critical for reproducibility in High-Throughput Screening (HTS)?
Maintaining a consistent thermal environment is paramount because biological and biochemical assays are highly sensitive to temperature fluctuations. Small variations can alter reaction rates, enzyme kinetics, and molecular binding interactions, leading to significant data variability and challenges in replicating results across experiments or between laboratories [54]. Thermodynamic parameters describing molecular interactions, such as binding affinity, are themselves temperature-dependent [55].
What are the primary sources of thermal variation in an HTS instrument?
Thermal variation can arise from several sources, including:
- Proximity to external ambient temperatures.
- The introduction of room-temperature samples into the system.
- Heat generated by other instrument components, such as agitation motors, vortexers, and centrifuges [54].
- Incompatible buffer additives in assays like Differential Scanning Fluorimetry (DSF) that can increase background noise [56].
What is a Thermal Shift Assay (TSA) and how is it used in drug discovery?
Thermal Shift Assays (TSAs), including Differential Scanning Fluorimetry (DSF) and the Cellular Thermal Shift Assay (CETSA), are label-free techniques used to measure direct interactions between a small molecule and its target protein. They work on the principle that a protein's thermal stability (its "melting temperature" or Tm) often increases when a drug molecule binds to it. This makes them invaluable for target engagement studies, from initial hit identification to validation in physiologically relevant cellular environments [56].
Troubleshooting Common Temperature-Related Issues
Issue: Inconsistent results across replicate wells in a microplate.
| Possible Cause | Solution |
|---|---|
| Temperature gradients across the plate | Ensure the instrument's thermal block is properly calibrated and operates within a tight distribution (e.g., 34.5 ±0.5 °C) [54]. Use plates with good thermal conductivity. |
| Evaporation in edge wells | Use a plate seal or a lid designed to prevent evaporation. Employing a humidified chamber for long-term assays can also mitigate this. |
| Sample solvent effects | Dissolve samples in the starting mobile phase or a solvent matched to the assay buffer to avoid temperature mismatches and unwanted solvent-strength effects [57]. |
Issue: High background noise or irregular melt curves in a DSF experiment.
| Possible Cause | Solution |
|---|---|
| Compound-dye interactions or intrinsic fluorescence | Test compounds alone with the dye to identify interference. Consider using a different fluorescent dye or an alternative detection method [56]. |
| Incompatible buffer components | Avoid detergents or viscosity-increasing additives that can raise background fluorescence. Optimize the buffer for compatibility with the DSF dye [56]. |
| Compound solubility issues | Ensure compounds are fully dissolved in the assay buffer. Precipitation can cause light scattering and irregular curve shapes [56]. |
Issue: No observed thermal shift in a cellular thermal shift assay (CETSA).
| Possible Cause | Solution |
|---|---|
| Poor cell membrane permeability | The test compound may not be efficiently crossing the cell membrane. Verify permeability or use a cell-lysed CETSA format to bypass this barrier [56]. |
| Insufficient compound concentration or incubation time | Ensure the incubation period is long enough for the compound to enter the cell and bind its target, but not so long that phenotypic effects dominate [56]. |
| Low protein abundance | Use a sensitive detection method (e.g., western blot with a high-quality antibody) to ensure the target protein signal is detectable above the background [56]. |
Performance Data & Metrics
Key Performance Metrics for Robust HTS Assays
A successful high-throughput screening assay must balance sensitivity, reproducibility, and scalability. The following table summarizes key metrics to evaluate assay performance, particularly regarding temperature stability and data quality [58].
| Metric | Ideal Value | Significance for Reproducibility |
|---|---|---|
| Z'-factor | 0.5 – 1.0 | Indicates an excellent assay with a large separation between positive and negative controls. A high Z'-factor is critical for reliable hit identification. |
| Signal-to-Noise Ratio (S/N) | As high as possible | Measures the strength of the assay signal relative to background noise. Temperature fluctuations can significantly increase noise. |
| Coefficient of Variation (CV) | < 10% | Measures the precision (well-to-well and plate-to-plate variability). A low CV is a direct indicator of assay robustness and reproducibility. |
| Temperature Uniformity | e.g., ±0.25 °C | The 6-sigma distribution of temperatures across a system should fall within a very tight range to ensure consistent reaction conditions for every well [54]. |
Experimental Protocols
Protocol: Thermal Profiling of an HTS Instrument
Purpose: To locate and quantify all contributing heat sources within a diagnostic or HTS instrument, identifying potential causes of thermal variation that impact assay reproducibility [54].
Methodology:
- Placement of Probes: Strategically place calibrated thermal probes across the instrument, focusing on areas near heat-generating components (motors, Peltier elements) and the sample plate itself.
- Data Logging: Operate the instrument under normal run conditions while logging temperature data from all probes in real-time.
- Root Cause Analysis: Analyze the thermal profile to identify components causing local temperature fluctuations.
- Design Optimization: Implement hardware design changes to minimize impacts. For example, a motor plate skewing temperatures upward can be re-engineered to provide required torque at a lower current, thereby reducing heat output [54].
Protocol: Differential Scanning Fluorimetry (DSF) for Target Engagement
Purpose: To identify small molecules that bind to a purified recombinant protein by measuring shifts in the protein's melting temperature (Tm) [56].
Workflow:
- Sample Preparation: In a multi-well plate, mix the purified protein with a polarity-sensitive fluorescent dye (e.g., SyproOrange) and the test compound.
- Temperature Ramp: Place the plate in a real-time PCR instrument or thermal cycler and heat the sample gradually (e.g., from 25°C to 95°C at a rate of 1°C/min).
- Fluorescence Measurement: As the temperature increases, the dye binds to hydrophobic regions of the protein exposed during unfolding, causing a fluorescence increase.
- Data Analysis: Plot fluorescence vs. temperature to generate a melt curve. The Tm is the midpoint of the protein unfolding transition. A positive shift in Tm (ΔTm) in the presence of a compound indicates stabilization due to binding.
The diagram below illustrates the logic and workflow of a DSF experiment.
The Scientist's Toolkit: Research Reagent Solutions
Key Reagents for Thermal Stability Assays
| Item | Function |
|---|---|
| Polarity-Sensitive Dye (e.g., SyproOrange) | A fluorescent dye that is quenched in aqueous solution but fluoresces brightly when bound to hydrophobic protein patches exposed during thermal unfolding. It is the core detection reagent in DSF [56]. |
| Recombinant Target Protein | A purified protein of interest, essential for biochemical TSAs like DSF and the Protein Thermal Shift Assay (PTSA) [56]. |
| Heat-Stable Loading Control Protein (e.g., SOD1) | Used in PTSA and CETSA for data normalization. A protein that remains stable at high temperatures, allowing for accurate quantification of the target protein's melting behavior [56]. |
| Validated Antibody for Target Protein | Critical for detecting the specific target protein in western blot-based readouts for PTSA and CETSA experiments [56]. |
| Universal Biochemical Assay Kits (e.g., Transcreener) | Homogeneous, mix-and-read assays that use fluorescence to detect biochemical activity (e.g., ADP formation for kinases). They are flexible, robust, and well-suited for HTS campaigns to test for potency and residence time [58]. |
System-Level Solutions for Thermal Management
The diagram below outlines a comprehensive engineering approach to achieving precise thermal control in automated instruments, directly addressing reproducibility challenges [54].
The inability to reproduce research results is a frequent and costly stumbling block in drug discovery, with one analysis suggesting approximately 50% of published biomedical research is not reproducible, costing an estimated $50 billion annually in the United States alone [59]. In high-throughput screening (HTS), the hit triage process—where active compounds (hits) from primary screens are evaluated and prioritized—represents a critical juncture for addressing these reproducibility challenges. The fundamental goal of hit triage is to strategically balance the elimination of false positives (compounds that appear active due to assay interference or other artifacts) while minimizing the risk of falsely excluding genuine hits (false negatives) [47] [60]. This balance is essential for building a reproducible pipeline in early drug discovery, as decisions made during hit triage determine which chemical starting points progress toward further development and eventual therapeutics.
Frequently Asked Questions (FAQs)
Q1: Why is hit triage particularly challenging in high-throughput screening? Hit triage is challenging because most HTS campaigns generate a high percentage of false positive hits. A primary HTS campaign screening 500,000 compounds with a 1-2% hit rate typically yields 5,000-10,000 actives, many of which are false positives resulting from various forms of assay interference rather than genuine biological activity [60]. These false positives can arise from compound aggregation, fluorescence interference, chemical reactivity, or interference with specific assay detection technologies [47] [60].
Q2: What are the most common sources of false positives in biochemical HTS assays? Common sources of false positives include:
- Assay technology interference: Fluorescent compounds causing autofluorescence or signal quenching, inner filter effects from light absorption, and singlet oxygen quenching in assays like AlphaScreen [60].
- Compound-mediated interference: Chemical aggregation, promiscuous inhibitors, redox-active compounds, and chelators [47].
- Protein-tag interference: Compounds that interfere with affinity matrices binding to protein tags (e.g., His-tag binders in AlphaScreen technology) [60].
Q3: How can we minimize the risk of discarding genuine hits during triage? Minimizing false negatives requires:
- Implementing multiple orthogonal assays with different detection technologies
- Using dose-response confirmation rather than single-point measurements
- Applying chemoinformatics filters judiciously rather than as absolute rules
- Maintaining comprehensive records of all triage decisions for future re-analysis
- Establishing statistically robust hit-calling criteria that don't exclude moderately active compounds [47] [60]
Q4: What documentation practices support reproducible hit triage? Reproducible practices include maintaining electronic laboratory notebooks, detailed protocol documentation, version control for analysis code, and recording all data processing steps. Computational methods should document software versions, parameters, and specific algorithms used. Sharing Jupyter notebooks with both code and explanatory text facilitates reproducibility and collaboration [61].
Troubleshooting Guides
Problem: High False Positive Rate in Primary Screening
Symptoms:
- High initial hit rate (>3-5%) with poor confirmation rate (<70%)
- Inconsistent activity in dose-response curves
- Unusual dose-response curve shapes (e.g., bell-shaped, shallow, or extremely steep)
Solutions:
- Implement counter assays to identify technology-specific interferers:
- For fluorescence-based assays: include fluorescence quenching/enhancement counterscreens
- For tag-based systems (e.g., His-tag): test different affinity tags where possible
- Include detergent or BSA in assays to counteract nonspecific binding or aggregation [47]
Apply computational filters strategically:
- Use PAINS (pan-assay interference compounds) filters to flag potentially promiscuous compounds
- Implement additional target-specific interference filters (e.g., His-tag interference filters)
- Analyze historical screening data to identify frequent hitters [60]
Optimize assay conditions:
- Validate assay robustness using metrics like Z'-factor (>0.5) before primary screening
- Include appropriate controls in every plate
- Use optimized buffer conditions to reduce nonspecific effects [47]
Problem: Inconsistent Results Across Replicate Experiments
Symptoms:
- Poor correlation between technical or biological replicates
- Low statistical power in confirmation assays
- Inability to reproduce original screening results in follow-up experiments
Solutions:
- Address technical variability:
- Standardize reagent sources, preparation methods, and handling procedures
- Implement plate randomization schemes to avoid positional effects
- Use validated, high-quality reagents with proper QC documentation [59]
Improve statistical power:
- Ensure adequate sample sizes through proper power analysis
- Implement appropriate replication schemes (technical vs. biological)
- Use statistical methods that account for missing data in reproducibility assessment [6]
Enhance protocol documentation:
- Record detailed experimental protocols including all critical parameters
- Maintain comprehensive records of reagent batch numbers and preparation dates
- Use electronic lab notebooks for better documentation and searchability [61]
Problem: Distinguishing Genuine Hits from Assay Artifacts
Symptoms:
- Compounds show activity in primary assay but not in orthogonal formats
- Discrepancy between biochemical and cellular activity
- Unusual structure-activity relationships (SAR)
Solutions:
- Implement orthogonal assay strategies:
- Confirm activity using different detection technologies (e.g., luminescence vs. fluorescence)
- Use biophysical methods (SPR, ITC, MST) for binding confirmation in target-based approaches
- Apply high-content imaging to move beyond bulk population measurements [47]
Conduct cellular fitness assessment:
- Test for general toxicity using viability assays (CellTiter-Glo, MTT)
- Assess specific cytotoxicity mechanisms (apoptosis, membrane integrity)
- Use multiparameter assays like cell painting for comprehensive morphological profiling [47]
Perform mechanistic counterscreening:
- Test compounds against related but distinct targets for selectivity assessment
- Use engineered cell lines or isogenic controls for pathway specificity
- Evaluate target engagement using cellular thermal shift assays (CETSA) or other direct target-binding methods [60]
Experimental Protocols & Workflows
Comprehensive Hit Triage Workflow
The following diagram illustrates the strategic workflow for hit triage that systematically balances false positive reduction with false negative risk management:
Detailed Experimental Protocols
Protocol 1: Dose-Response Confirmation Assay
Purpose: To verify primary screening hits and quantify compound potency through concentration-response relationships.
Materials:
- Compound plates (serial dilutions of primary hits)
- Assay reagents (identical to primary screening conditions)
- Positive and negative controls
- 384-well microtiter plates
- Liquid handling robotics or multichannel pipettes
- Plate reader appropriate for detection method
Procedure:
- Prepare compound serial dilutions in DMSO (typically 1:3 or 1:2 dilution series across 10 concentrations)
- Transfer compounds to assay plates using acoustic dispensing or pin tools, maintaining final DMSO concentration ≤1%
- Add assay reagents according to optimized primary screening protocol
- Incubate under appropriate conditions (time, temperature)
- Measure signal using validated detection method
- Include controls on each plate: positive control (100% inhibition), negative control (0% inhibition), and vehicle control (DMSO only)
Data Analysis:
- Calculate % inhibition/activation for each concentration relative to controls
- Fit dose-response curves using four-parameter logistic model
- Determine IC50/EC50 values and curve quality metrics (R², Hill slope)
- Flag compounds with poor curve fit (R² < 0.8), unusual Hill slopes (<0.5 or >2.5), or incomplete efficacy (<70% max response) for further scrutiny [47]
Protocol 2: Orthogonal Assay Implementation
Purpose: To confirm compound activity using different detection technology or experimental format.
Materials:
- Active compounds from dose-response confirmation
- Alternative detection system (e.g., luminescence vs. fluorescence)
- Assay-specific reagents for orthogonal format
- Appropriate plate reader or detection instrument
Procedure:
- Select orthogonal format based on primary assay:
- For binding assays: Implement SPR, ITC, or MST
- For enzymatic assays: Switch detection method (e.g., fluorescence to luminescence)
- For cell-based assays: Use different readout (e.g., reporter gene vs. high-content imaging)
- Prepare compounds and reagents for orthogonal format
- Run orthogonal assay with appropriate controls
- Compare activity profiles between primary and orthogonal formats
Interpretation:
- Genuine hits: Show consistent activity across multiple assay formats
- Technology-specific artifacts: Active only in primary assay format
- Context-dependent artifacts: Show differential activity in biochemical vs. cellular assays [47]
Data Presentation & Analysis
Quantitative Comparison of Hit Triage Assay Types
Table 1: Comparison of Experimental Approaches for Hit Triage
| Assay Type | Primary Purpose | Typical Exclusion Rate | Key Strengths | Common Limitations |
|---|---|---|---|---|
| Counter Assays | Identify technology-specific interference | 20-40% | Directly addresses assay artifacts; high throughput | May exclude some genuine hits; requires careful design |
| Orthogonal Assays | Confirm biological activity | 30-50% | Confirms true biological activity; reduces false positives | Often lower throughput; more resource intensive |
| Cellular Fitness Assays | Exclude general toxicity | 10-25% | Identifies cytotoxic compounds early; improves compound quality | May exclude compounds with specific therapeutic toxicity |
| Selectivity Profiling | Assess target specificity | 20-35% | Identifies promiscuous inhibitors; improves specificity | Requires multiple related targets; resource intensive |
| Chemoinformatics Filters | Computational triage | 15-30% | Rapid and inexpensive; applicable early in process | Risk of over-filtering; may perpetuate historical biases |
Statistical Assessment of Reproducibility
Methods for Evaluating Assay Reproducibility:
For high-throughput experiments with significant missing data (e.g., dropout in single-cell RNA-seq), traditional correlation measures (Pearson/Spearman) can be misleading when excluding zero values. The Correspondence Curve Regression (CCR) method accounts for missing values in reproducibility assessment by modeling the probability that a candidate consistently passes selection thresholds across replicates [6].
Key Metrics:
- Z'-factor: Measures assay quality and separation between positive and negative controls (>0.5 recommended for robust assays)
- Signal-to-noise ratio: Should be >5 for reliable detection of active compounds
- Coefficient of variation (CV): Should be <20% for replicate measurements
- Reproducibility rate: Percentage of hits confirmed in repeat testing (>70% target) [60]
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for Hit Triage Operations
| Reagent/Material | Function in Hit Triage | Quality Considerations | Example Applications |
|---|---|---|---|
| Validated Compound Libraries | Source of chemical starting points | Purity >90%; structural diversity; known storage history | Primary screening; structure-activity relationships |
| Cell Line Authentication | Biologically relevant assay system | Regular mycoplasma testing; STR profiling; passage number monitoring | Cell-based assays; phenotypic screening |
| Tag-Specific Affinity Matrices | Protein detection in binding assays | Lot-to-lot consistency; binding capacity validation | AlphaScreen; TR-FRET; pull-down assays |
| Counter Assay Reagents | Identify technology interference | Signal dynamic range optimization; interference controls | Fluorescence quenching; tag displacement assays |
| Viability Assay Kits | Assess cellular fitness | Linear range validation; compatibility with primary readout | Cytotoxicity assessment; general cellular health |
| High-Quality DMSO | Compound solvent | Low water content; peroxide-free; sterile filtered | Compound storage and dilution; vehicle controls |
Effective hit triage requires both rigorous experimental design and a cultural commitment to reproducibility throughout the research organization. This includes thorough documentation practices, mentorship in experimental design, statistical training for proper power analysis, and institutional support for the time and resources required for adequate validation [59] [61]. By implementing the systematic approaches outlined in this guide—strategic assay selection, appropriate use of computational filters, and comprehensive validation cascades—research teams can significantly improve the reproducibility of their hit triage outcomes. This systematic approach to balancing false positive reduction with false negative risk management ultimately enhances the efficiency of the entire drug discovery pipeline, increasing the likelihood that research investments will translate into viable therapeutic candidates.
Frequently Asked Questions (FAQs)
Q1: What are the primary causes of poor reproducibility in high-throughput microscopy? Poor reproducibility often stems from batch effects, such as variations in cell culture conditions, reagent lots, or environmental factors across different experiment dates. Additionally, inconsistent image analysis due to poorly segmented cells or inadequate validation of machine learning models can significantly impact results. Implementing robust automated workflows and careful experimental design is crucial to mitigate these issues [62].
Q2: How can I determine if my dataset is large enough for training a reliable deep learning model? The required dataset size depends on the complexity of your phenotypic assay and the model you are training. One study found that reducing the number of training images from 1137 to 176 led to a 12-fold increase in Mean Squared Error (MSE), from 4,335.99 to 49,973.52, for a cell counting task [63]. It's essential to use performance metrics like MSE on a held-out test set to evaluate if your model has learned generalizable patterns. If error rates are high, increasing your dataset size or employing data augmentation is likely necessary.
Q3: My bright-field live-cell images have low contrast and are noisy. What segmentation approach should I use? Conventional tools like Cellpose may perform poorly on challenging bright-field images [64]. A robust solution is a CNN-based pipeline (e.g., U-Net) enhanced with attention mechanisms and instance-aware systems, which has been shown to achieve up to 93% test accuracy and an 89% F1-score on low-contrast, noisy bright-field images. Incorporating adaptive loss functions and hard-instance retraining can further improve performance on difficult samples [64].
Q4: What metrics should I use to validate the reproducibility of my screening assay? Beyond the commonly used Z'-factor for assay quality [41], consider statistical methods designed for high-throughput data. Correspondence Curve Regression (CCR) is a powerful method that assesses how operational factors affect reproducibility across a range of selection thresholds, and it can be extended to handle missing data common in technologies like single-cell RNA-seq [6].
Q5: How can I ensure my deep learning model learns biological phenotypes and not experimental artifacts? Use a robust experimental design that controls for potential confounds. This includes:
- Balanced Plate Layouts: Alternate case and control lines on the same plate [62].
- Multiple Batch Runs: Conduct several identical experimental batches to ensure consistency [62].
- Covariate Analysis: Perform statistical tests (e.g., lasso variable selection) to confirm that your model's predictions are not biased by technical factors like plating date or well location [62].
Troubleshooting Guides
Issue 1: High Variation in Cell Counts Between Replicate Assay Plates
Problem: Inconsistent cell counts after seeding, leading to unreliable data.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Inconsistent cell culture | Check growth rates during expansion; look for variations in confluence or morphology. | Implement automated, highly standardized procedures for cell thawing and expansion to minimize manual handling variation [62]. |
| Automated liquid handler malfunction | Calibrate liquid handling instruments and check for clogged tips. Verify dispensed volumes gravimetrically. | Perform regular preventative maintenance and include dispensing verification steps in the workflow [41]. |
Issue 2: Poor Performance of a Pre-trained Segmentation Model on New Images
Problem: A model that worked well on one set of images fails when applied to new data from a slightly different condition.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Domain shift (e.g., different microscope, cell line, or staining intensity) | Compare basic image statistics (e.g., average intensity, contrast) between the old and new datasets. | Fine-tune the pre-trained model on a small set of annotated images from the new domain. Consider using a model trained for cross-modality robustness [64]. |
| Inadequate ground truth | Manually inspect a subset of the model's predictions and the original ground truth masks. | Generate high-quality, manual ground truth annotations specifically for your challenging images, as automated tools can be unreliable [64]. |
Issue 3: Machine Learning Model Fails to Generalize Across Experimental Batches
Problem: A model trained to detect a disease phenotype performs well on its training batch but fails on data from a new experiment.
Solution: Implement a rigorous cross-validation strategy.
- Stratify by Batch: Instead of a random train-test split, use a batch-out cross-validation scheme. Train your model on data from three batches and test its performance on the held-out fourth batch [62].
- Validate on New Individuals: For disease modeling, ensure that the model is tested on cell lines from donors that were not present in the training data at all. This assesses its ability to generalize to new individuals [62].
- Leverage Deep Embeddings: Use fixed weights from a pre-trained convolutional neural network (e.g., on ImageNet) to generate deep embeddings from your images. These embeddings can be more robust for training machine learning models than hand-crafted features [62].
Quantitative Data for Experimental Benchmarking
Table 1: Segmentation Model Performance Across Cell Lines
Performance of a CNN model for cell quantification in digital contrast microscopy images, measured by Mean Squared Error (MSE). A lower MSE indicates better performance [63].
| Cell Line | MSE (Large Image Set) | MSE (Small Image Set) | Best Model Correlation (R) |
|---|---|---|---|
| A549 | 4,335.99 | 49,973.52 | 0.953 (Strong Positive) |
| Huh7 | 25,295.23 | 79,473.88 | 0.821 (Positive) |
| 3T3 | 36,897.03 | 52,977.05 | 0.100 (No Correlation) |
Table 2: Comparison of Segmentation Tools for Bright-Field Microscopy
A comparison of different segmentation methodologies highlights trade-offs between performance and practicality [64].
| Method / Tool | Key Principle | Reported Performance | Practical Considerations |
|---|---|---|---|
| Proposed CNN Pipeline | U-Net with attention, instance-aware systems, adaptive loss. | 93% accuracy, 89% F1-score on bright-field. | Competitive accuracy, designed for lab deployment, minimal compute power. |
| Self-Supervised Learning | Optical flow-based pseudo-labeling (annotation-free). | F1-score 0.77–0.88 on fluorescence. | Failed on 60% of low-contrast samples; slow (50-60 sec/image). |
| Cellpose-SAM | Integrates Segment Anything Model (SAM) with flow decoding. | 15% IoU improvement on phase-contrast. | Poor performance on bright-field; high VRAM (16 GB) required. |
Standard Experimental Protocols
Protocol 1: An Unbiased Workflow for Phenotypic Profiling of Patient Fibroblasts
This protocol, adapted from a study on Parkinson's disease, is designed for robustness and reproducibility in identifying disease signatures [62].
Detailed Methodology:
- Cell Line Selection & Quality Control: Select patient and matched healthy control lines. Subject all lines to thorough genetic quality control and exclusion criteria [62].
- Automated Cell Culture: Use a modular robotic platform (e.g., NYSCF Global Stem Cell Array) for highly standardized, automated cell thawing, expansion, and seeding into assay plates. This minimizes manual variation [62].
- Robust Assay Plate Design: To control for location bias, use a plate layout that alternates patient and control lines in adjacent wells. Pair lines by age and sex where possible. Run multiple batches with replicates of each layout [62].
- Multiplexed Staining and Imaging: Two days after seeding, stain cells automatically using the Cell Painting assay. This multiplexed panel uses fluorescent dyes to label five cellular compartments: nucleus (DAPI), nucleoli and cytoplasmic RNA, endoplasmic reticulum, actin and golgi, and mitochondria. Image plates in all five channels [62].
- Deep Learning-Based Image Analysis:
- Feature Extraction: Pass images through a pre-trained deep convolutional neural network (e.g., Inception) to generate deep embeddings—lower-dimensional morphological profiles of the images.
- Model Training and Validation: Train machine learning models (e.g., Random Forest, Logistic Regression) on the well-averaged deep embeddings. Use a k-fold cross-validation scheme stratified by batch or individual donor to ensure the model generalizes to new experiments and new people [62].
Protocol 2: CNN-Based Segmentation of Challenging Bright-Field Live-Cell Images
This protocol is tailored for segmenting unstained live cells imaged with bright-field microscopy, where low contrast and noise are major challenges [64].
Detailed Methodology:
- Image Acquisition and Ground Truth Creation: Acquire bright-field microscopy images of live cells. Due to the poor performance of automated tools on difficult images, create high-quality manual ground truth segmentation masks for training and validation [64].
- Model Design: Implement a U-Net-like architecture with the following enhancements:
- Use a frozen encoder backbone pre-trained on a large dataset.
- Incorporate attention mechanisms to help the model focus on relevant cellular structures.
- Add instance-aware systems to better separate touching cells [64].
- Advanced Training Strategy:
- Use adaptive loss functions that are robust to class imbalance.
- Implement hard-instance retraining, where the model is subsequently trained on the samples it initially got wrong.
- Use a dynamic learning rate and progressive mechanisms to prevent overfitting [64].
- Ensemble and Validate: Use an ensemble technique (combining multiple models) for the final prediction. Validate the model on a held-out test set, reporting accuracy and F1-score. Perform a post-segmentation morphometric analysis (e.g., measuring cell area, circularity, aspect ratio) to extract biological insights [64].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents for High-Content Imaging and Cell Painting
Essential materials for setting up a robust, unbiased phenotypic screening platform [62].
| Item | Function / Application |
|---|---|
| Cell Painting Dye Set | A multiplexed fluorescent dye kit to label key cellular compartments: DAPI (nucleus), RNAs (nucleoli/cytoplasm), ER, Actin & Golgi (AGP), and Mitochondria (MITO). This provides a rich, unbiased morphological profile [62]. |
| Automated Cell Culture System | A robotic platform (e.g., Global Stem Cell Array) for standardized cell thawing, expansion, and seeding. Critical for minimizing batch-to-batch variation [62]. |
| High-Content Imager | An automated microscope capable of capturing high-resolution images in multiple fluorescent channels from multi-well plates [62]. |
| Pre-trained CNN Model Weights | Fixed weights from a deep neural network (e.g., trained on ImageNet). Used for transfer learning to generate powerful deep embeddings from cellular images without training a model from scratch [62]. |
| OMERO Data Management | An open-source data management system for storing, managing, and linking images, analytical data, and experimental metadata. Ensures reproducibility and community-wide access [65]. |
FAQs: Troubleshooting Common ICC Issues
FAQ 1: What are the primary causes of high background staining in ICC, and how can I reduce it?
High background, or non-specific signal, is a common issue that can obscure your results. The causes and solutions are multifaceted [66].
- Antibody Concentration: Too high a concentration of your primary or secondary antibody is a frequent culprit. Solution: Titrate your antibodies to find the optimal dilution that provides a strong specific signal with minimal background [67] [68].
- Insufficient Blocking: Inadequate blocking allows antibodies to bind non-specifically to sites in the sample. Solution: Increase the concentration of your blocking agent (e.g., normal serum or BSA) and/or extend the blocking incubation time. Ensure the normal serum used for blocking is from the same species as the host of the secondary antibody [69] [70].
- Incomplete Washing: Residual unbound antibodies can contribute to background. Solution: Increase the number and duration of wash steps after antibody incubations. Adding a gentle detergent like Tween-20 to your wash buffer and using gentle agitation can improve washing efficiency [67] [70].
- Non-Specific Fc Receptor Binding: Cells expressing Fc receptors can bind the constant region (Fc) of antibodies. Solution: Use Fc receptor blocking reagents or include normal serum from an appropriate species in your blocking buffer [71] [66].
- Fixative-Induced Autofluorescence: Aldehyde-based fixatives can cause autofluorescence. Solution: Quench fixed samples with a solution such as 0.1% sodium borohydride (NaBH4) in PBS [70].
FAQ 2: I am getting weak or no signal in my experiment. What steps should I take?
A lack of expected staining requires a systematic investigation of your protocol and reagents.
- Antibody Application: The most common cause is insufficient primary antibody binding. Solution: Increase the concentration of your primary antibody or extend the incubation time. Perform an antibody titration experiment to determine the ideal working concentration. Also, confirm that your primary and secondary antibodies are compatible [67] [68].
- Permeabilization: If your target is intracellular and you used a cross-linking fixative like paraformaldehyde, the cell membrane may not be adequately permeabilized for antibody entry. Solution: Ensure a permeabilization step with a detergent like Triton X-100 is included. Note that methanol fixation also permeabilizes cells, making a separate step unnecessary [69] [68].
- Antigen Availability: The target epitope might be masked due to over-fixation or the fixation method itself. Solution: Reduce fixation time or test alternative fixatives. For aldehyde-fixed samples, consider an antigen retrieval step, such as heating the sample in a citrate-based or urea buffer [67] [70].
- Antibody Specificity and Viability: Confirm that the antibody is validated for ICC and recognizes the native form of the protein. Also, improper antibody storage or repeated freeze-thaw cycles can degrade antibodies. Solution: Aliquot antibodies to avoid freeze-thaw damage and store them according to the manufacturer's recommendations [68] [70].
- Protein Expression: Verify that your target protein is expressed in the cell line you are using at detectable levels. Solution: Run a positive control with a cell line or sample known to express the protein abundantly [67] [68].
FAQ 3: How can I improve the reproducibility of my ICC assays, especially in a high-throughput screening context?
Reproducibility is critical for robust data, particularly in high-throughput settings [72].
- Standardize Cell Culture and Seeding: In high-throughput screening, ensure uniform cell distribution by using a reproducible single-cell dissociation protocol, such as treatment with Accutase, and seed a consistent number of cells in each well. Using a robust cell density prevents multilayered growth and ensures even staining [72].
- Automate and Minimize Variables: Where possible, use automated liquid handlers for reagent dispensing and washing to reduce human error. Employing automated imaging systems with predefined settings ensures consistent image acquisition across all samples [72] [73].
- Implement Rigorous Controls: Include both positive and negative controls in every experiment. For example, a well-defined control compound (like FGF2 for self-renewal or BMP4 for differentiation in stem cell assays) should be used to normalize data between plates and runs [72].
- Validate Your Antibodies: Use antibodies that have been rigorously validated for ICC. Strategies include using genetic approaches (e.g., CRISPR/Cas9 knockout cells) to confirm the absence of signal, or correlating signals with orthogonal methods like Western blotting [73].
- Use a Master Validation Protocol: For antibody validation, employ a standardized, high-throughput microscopy (HTM) workflow. Seed cells in multi-well plates, use automated imaging, and analyze images with unbiased, automated software like CellProfiler to quantify fluorescence intensity and subcellular localization [73].
Table 1: Summary of Common ICC Problems and Solutions
| Problem | Primary Causes | Recommended Solutions |
|---|---|---|
| High Background | Antibody concentration too high; Insufficient blocking; Inadequate washing [67] [66]. | Titrate antibodies; Increase blocking agent concentration/time; Increase wash number/duration with detergent [69] [70]. |
| Weak/No Signal | Low antibody binding; Inadequate permeabilization; Epitope masking [67] [68]. | Increase primary antibody concentration/time; Optimize permeabilization; Perform antigen retrieval [68] [70]. |
| Non-Specific Staining | Antibody cross-reactivity; Reactive aldehyde groups [66] [70]. | Include species-specific blocking; Use NaBH4 to quench autofluorescence [70]. |
| Cell Detachment | Harsh washing; Poor adherence [68] [70]. | Wash gently; Coat coverslips with poly-lysine [69] [68]. |
Experimental Protocols for Key Applications
Detailed ICC Protocol for General Use
This protocol is a reliable foundation for most ICC experiments, based on a standard methodology [69].
Materials:
- Cells and Coverslips: Sterile glass coverslips, optionally coated with poly-lysine for better adhesion.
- Fixative: Freshly prepared 4% paraformaldehyde (PFA) in PBS or ice-cold methanol.
- Permeabilization Buffer: 0.5% Triton X-100 in PBS (not needed if using methanol fixation).
- Blocking Buffer: 1-5% normal serum or BSA in PBS.
- Antibody Dilution Buffer: 1% normal serum or BSA in PBS.
- Primary Antibody: Specific to your target.
- Secondary Antibody: Fluorochrome-conjugated, raised against the species of the primary antibody.
- Mounting Medium: With DAPI and antifade agent.
Methodology:
- Cell Culture: Seed cells on sterile coverslips and grow to semi-confluency. Handle cells gently to avoid detachment.
- Fixation:
- Wash cells gently with room temperature PBS.
- Incubate in 4% PFA for 10 minutes at room temperature or in -20°C methanol for 10 minutes.
- Wash with PBS for 2 minutes.
- Permeabilization: (If using PFA) Incubate in 0.5% Triton X-100 for 5 minutes at room temperature. Wash with PBS for 5 minutes.
- Blocking: Incubate coverslips in blocking buffer for 1 hour at room temperature to reduce background.
- Primary Antibody Incubation:
- Prepare primary antibody in antibody dilution buffer.
- Incubate coverslips with the antibody for 1 hour at room temperature or overnight at 4°C.
- Wash three times with PBS for 5 minutes each.
- Secondary Antibody Incubation:
- Prepare fluorochrome-conjugated secondary antibody in antibody dilution buffer.
- Incubate coverslips for 1 hour at room temperature in the dark.
- Wash three times with PBS for 5 minutes each in the dark.
- Mounting and Imaging:
- Counterstain nuclei with DAPI or Hoechst if not present in the mounting medium.
- Invert coverslip onto a slide with a drop of mounting medium.
- Seal with nail polish if required and image with a fluorescence microscope.
High-Throughput Screening (HTS) ICC Protocol for hESCs
This protocol adapts ICC for a high-throughput screening context using human embryonic stem cells (hESCs), a technically challenging system [72].
Materials:
- Cells: hESCs maintained under feeder-free conditions.
- Dissociation Reagent: Accutase for single-cell dissociation.
- Plates: Matrigel-coated 384-well plates suitable for automated imaging.
- Automation Equipment: Liquid handling robots and a high-throughput laser scanning confocal microscope (e.g., GE InCell Analyzer 3000).
Methodology:
- Cell Preparation and Plating:
- Dissociate hESCs into a single-cell suspension using Accutase.
- Plate cells in Matrigel-coated 384-well plates at a uniform, optimized density (e.g., 6000 cells/well). This density should prevent multilayering and be suitable for automated analysis after 7 days.
- Cell Recovery and Compound Addition:
- Culture cells in conditioned medium for 48 hours to allow recovery from dissociation.
- At the 48-hour mark, change the medium and add small molecule compounds from your library (e.g., at 10µM final concentration). Withdraw known maintenance factors like FGF2 to create a "sensitized" state for the assay.
- Incubation and Fixation:
- Incubate cells with compounds for a defined period (e.g., 5 days).
- Fix and permeabilize cells according to your standard ICC protocol (see above), ideally using an automated platform.
- Immunostaining and Analysis:
- Perform automated immunostaining for your target readout (e.g., pluripotency marker Oct4).
- Counterstain nuclei with Hoechst 33342.
- Acquire images using the high-throughput microscope.
- Normalize the target signal (e.g., Oct4 intensity) to the nuclear stain to control for cell number effects.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for ICC and HTS
| Reagent / Solution | Function / Application | Specific Example / Note |
|---|---|---|
| Accutase | Enzymatic dissociation for single-cell suspension. | Critical for uniform plating of sensitive cells like hESCs in HTS [72]. |
| Normal Serum | Blocking non-specific binding in ICC. | Should be from the same species as the secondary antibody host [69] [71]. |
| Fc Receptor Block | Reduces non-specific antibody binding via Fc receptors. | Essential for staining immune cells or other Fc receptor-expressing cells [71]. |
| Tandem Dye Stabilizer | Prevents degradation of tandem fluorophore conjugates. | Crucial for multi-color panels in flow cytometry and imaging to prevent signal spillover [71]. |
| Brilliant Stain Buffer | Mitigates dye-dye interactions in polymer-based fluorophores. | Used in highly multiplexed panels containing "Brilliant" dyes (e.g., BD Horizon) [71]. |
| Sodium Borohydride (NaBH₄) | Quenches autofluorescence caused by aldehyde fixatives. | Incubate fixed samples with 1% NaBH₄ in PBS; optimize time to preserve specific signal [70]. |
| Automated Imaging System | High-throughput, consistent image acquisition. | Systems like the GE InCell Analyzer 3000 enable HTS of multi-well plates [72]. |
| CellProfiler Software | Open-source software for automated image analysis. | Enables unbiased, quantitative analysis of fluorescence intensity and morphology [73]. |
Conclusion
Addressing reproducibility in high-throughput screening is not a single-step fix but requires a holistic strategy integrating foundational understanding, rigorous methodology, proactive troubleshooting, and comprehensive validation. The key takeaways are that precise environmental control, advanced automation, and intelligent data analysis are non-negotiable for robust HTS. Furthermore, moving beyond mere reproducibility to demonstrate analytical validity through known-truth simulations and orthogonal methods is paramount for scientific credibility. Future directions point towards greater integration of AI and machine learning for predictive modeling and hit selection, the adoption of more physiologically relevant 3D cellular models, and the development of universally accepted standardized validation protocols. By embracing these principles, the scientific community can enhance the reliability of HTS data, thereby accelerating the translation of discoveries into impactful clinical applications and building a more robust foundation for biomedical research.
References
- 1. What is High-Throughput Screening (HTS)? [https://www.labkey.com/high-throughput-screening-definition/]
- 2. Webinar Series on Quality and Reproducibility issues in ... [https://eatris.eu/news/webinar-series-quality-reproducibility-issues-drug-development/]
- 3. Process Validation and Screen Reproducibility in High- ... [https://www.sciencedirect.com/science/article/pii/S2472555222080182]
- 4. How Automation Overcomes Variability & Limitations in ... [https://dispendix.com/blog/how-automation-overcomes-variability-limitations-in-hts-troubleshooting]
- 5. Adaptation of High-Throughput Screening in Drug Discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3269696/]
- 6. Assessing Reproducibility of High-throughput Experiments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9039958/]
- 7. Top High Throughput Screening Software for Labs | Trends [https://www.scispot.com/blog/top-high-throughput-screening-software-for-labs]
- 8. High Throughput Screening Assays for Drug Discovery [https://bellbrooklabs.com/high-throughput-screening-assays-drug-discovery/?srsltid=AfmBOopKRJBr8lopG04AeyLZ0d1hkT_Z-n_HYJEUgDug3Q3CgVECF_gf]
- 9. High Throughput Screening (HTS) Services [https://www.evotec.com/solutions/drug-discovery-preclinical-development/discovery/hit-identification-services/high-throughput-screening-hts-services]
- 10. Spatial artifact detection improves the reproducibility of drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570324/]
- 11. Lot-to-Lot Variance in Immunoassays—Causes, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10252387/]
- 12. Managing Environmental Factors and Laboratory ... [https://www.msesupplies.com/blogs/news/managing-environmental-factors-and-laboratory-conditions-with-sper-scientific?srsltid=AfmBOooysnX3oVvTvxv3XgUNyyOpgzsyYO3UA_M3FlEZTZ8IAMc9crTw]
- 13. Measuring the Impact of Common Environmental ... [https://www.aicompanies.com/education-training/knowledge-center/measuring-the-impact-of-common-environmental-conditions-on-laboratory-data-integrity/]
- 14. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 15. How to Troubleshoot Experimental Protocols in the Lab [https://www.linkedin.com/advice/1/what-some-strategies-troubleshooting-experimental-jekfe]
- 16. Improving reproducibility of photocatalytic reactions —how to... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10770379/]
- 17. Improving reproducibility of photocatalytic reactions—how ... [https://www.nature.com/articles/s41467-023-44362-0]
- 18. Photochemical Reactor Setup - Photoreactor Setup and Design [https://hepatochem.com/photoreactors-leds-accessories/photoreactor-setup-and-design/]
- 19. What Makes a Good Photoreactor Design? [https://www.asynt.com/blog/good-photoreactor-design/]
- 20. High-throughput behavioral screening in Caenorhabditis ... [https://www.nature.com/articles/s41598-025-10370-x]
- 21. 10 Guidelines for DataViz Accessibility [https://www.highcharts.com/blog/tutorials/10-guidelines-for-dataviz-accessibility/]
- 22. Data Visualizations, Charts, and Graphs - Digital Accessibility [https://accessibility.huit.harvard.edu/data-viz-charts-graphs]
- 23. Data visualisation: colours - Government Analysis Function [https://analysisfunction.civilservice.gov.uk/policy-store/data-visualisation-colours-in-charts/]
- 24. From Patterns to Pills: How Informatics Is Shaping Medicinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114992/]
- 25. Making data visualizations accessible [https://www.tpgi.com/making-data-visualizations-accessible/]
- 26. Categorical schemes | D3 by Observable [https://d3js.org/d3-scale-chromatic/categorical]
- 27. Managing colors in d3.js [https://d3-graph-gallery.com/graph/custom_color.html]
- 28. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 29. Process validation and screen reproducibility in high ... [https://pubmed.ncbi.nlm.nih.gov/19171922/]
- 30. The Art of Troubleshooting for Customer Support ... [https://www.helpscout.com/helpu/art-of-troubleshooting-support/]
- 31. The complete guide to customer service troubleshooting [https://devrev.ai/blog/customer-service-troubleshooting]
- 32. Most Common Helpdesk Problems and How to Solve Them [https://www.alert-software.com/blog/the-most-common-helpdesk-problems-and-how-to-solve-them]
- 33. Designing High-Throughput Experiments Using Microplate ... [https://www.labx.com/resources/designing-high-throughput-experiments-using-microplate-technology/5576]
- 34. Advanced Assay Development Guidelines for Image-Based ... [https://www.ncbi.nlm.nih.gov/books/NBK126174/]
- 35. Navigating Challenges with Assay Plate Identification in ... [https://www.massbio.org/news/member-news/navigating-challenges-with-assay-plate-identification-in-drug-discovery/]
- 36. High-Throughput Screening Platforms and Robotics [https://www.labmanager.com/high-throughput-screening-platforms-and-robotics-34584]
- 37. Reducing Errors and Increasing Throughput in Drug ... [https://www.scientificlabs.co.uk/news/article/1790]
- 38. CHALLENGES IN SECONDARY ANALYSIS OF HIGH ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3976302/]
- 39. The future of robotics in the pharmaceutical industry. [https://www.essert.com/blog/robotics/future-robotics-pharmaceutical-industry/]
- 40. The automation revolution in drug discovery [https://www.ddw-online.com/the-automation-revolution-in-drug-discovery-33927-202503/]
- 41. High-Throughput Screening (HTS): A Simple Guide ... [https://www.chemcopilot.com/blog/hts-material-discovery]
- 42. Your liquid handling robot is broken. Or is it? (Part 2) [https://www.aicompanies.com/education-training/knowledge-center/your-liquid-handling-robot-is-broken-or-is-it-part-2/]
- 43. Automated Liquid Handlers As Sources of Error [https://www.bioprocessintl.com/assays/automated-liquid-handlers-as-sources-of-error]
- 44. Challenges and pitfalls of acoustic dispensing systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6812406/]
- 45. ExperimentAcousticLiquidHandli... [https://www.emeraldcloudlab.com/helpfiles/experimentacousticliquidhandling]
- 46. A Researcher's Guide to Optimizing High-throughput ... [https://www.ranomics.com/navigating-the-hurdles-a-researchers-guide-to-optimizing-high-throughput-screens-library-design-and-protein-engineering]
- 47. Brief Guide: Experimental Strategies for High-Quality Hit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293735/]
- 48. High Throughput Screening (HTS) [https://www.sygnaturediscovery.com/drug-discovery/bioscience/screening/medium-high-throughput-screening-mts-hts-2/]
- 49. High Throughput Screening [https://www.sygnaturediscovery.com/drug-discovery/bioscience/screening/high-throughput-screening-hts-2/]
- 50. Streamlined Chromatography Data Integration with ZONTAL [https://zontal.io/products/chromatography/]
- 51. Integrating AUROC and SSMD for quality control in ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629507/]
- 52. Strictly standardized mean difference [https://en.wikipedia.org/wiki/Strictly_standardized_mean_difference]
- 53. Quality by Design for Preclinical In Vitro Assay Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788254/]
- 54. Thermal Management in High-Throughput Screening [https://mls.ascentialtech.com/mls/resources/thermal-management-guide/]
- 55. Thermodynamic Studies for Drug Design and Screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC3496183/]
- 56. Thermal shift assays in drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S1056871925008007]
- 57. HPLC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/industrial/chromatography/chromatography-learning-center/high-performance-liquid-chromatography-hplc-support/hplc-troubleshooting.html]
- 58. High Throughput Screening Assays for Drug Discovery [https://bellbrooklabs.com/high-throughput-screening-assays-drug-discovery/?srsltid=AfmBOoreUxUY-0d5iDkKs-L4JEpeiy1PW2vT8HPqJ-BkZD_qhvB2zGmf]
- 59. Research Reproducibility: A Costly Stumbling Block for Drug ... [https://wewillcure.com/insights/therapeutics/research-reproducibility-a-costly-stumbling-block-for-drug-discovery]
- 60. The importance of adequately triaging hits from HTS ... [https://www.drugtargetreview.com/article/33749/the-importance-of-adequately-triaging-hits-from-hts-campaigns/]
- 61. Towards reproducible computational drug discovery [https://jcheminf.biomedcentral.com/articles/10.1186/s13321-020-0408-x]
- 62. Integrating deep learning and unbiased automated high ... [https://www.nature.com/articles/s41467-022-28423-4]
- 63. Cell quantification in digital contrast microscopy images ... [https://www.nature.com/articles/s41598-023-29694-7]
- 64. High-Throughput Low-Cost Segmentation of Brightfield ... [https://arxiv.org/html/2508.14106v1]
- 65. High-throughput Imaging as a versatile and unbiased ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6342277/]
- 66. Artifacts in IHC [https://www.biozol.de/en/techniques/Artifacts-in-IHC]
- 67. Immunocytochemistry Troubleshooting: ICC Help & ... [https://www.bio-techne.com/applications/imaging/immunocytochemistry/troubleshooting]
- 68. Immunocytochemistry Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunocytochemistry-troubleshooting/?srsltid=AfmBOop0BUwI-hAHzJ09Cld0fe5hp-57FAnbgmYzdzw64Pq17JPdKIoB]
- 69. Immunocytochemistry (ICC) Protocol [https://www.bio-techne.com/resources/protocols-troubleshooting/immunocytochemistry]
- 70. ICC/IF Troubleshooting [https://www.antibodies.com/applications/immunofluorescence/immunofluorescence-troubleshooting]
- 71. Optimization of the Blocking and Signal Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462741/]
- 72. HIGH-THROUGHPUT SCREENING ASSAY FOR THE ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2756729/]
- 73. High-throughput screening and validation of antibodies ... [https://www.nature.com/articles/s42003-021-01744-8]